CUHK
News Centre
CUHK Researchers Set New Direction with World’s First Study on Aspirin Use after Lower Gastrointestinal Hemorrhage
A recently published study led by the Faculty of Medicine at The Chinese University of Hong Kong (CUHK) showed that in patients with a history of aspirin-associated lower gastrointestinal (GI) bleeding, discontinuation of aspirin would lead to a 61% increase in serious cardiovascular events. It is the world’s first study to report significant findings to assist clinical decision making for these patients. It is suggested that physicians should critically evaluate individual patients’ cardiovascular risk before resuming aspirin therapy. The findings have been published in the leading medical journal Gastroenterology, and will be incorporated into the practice guidelines of various professional bodies in the United States.
Background
Aspirin is an important drug to treat cardiovascular diseases. In recent years, it has been increasingly used for prevention of coronary artery disease, stroke and colorectal cancer. While the side effects of aspirin to the stomach are well established, few doctors and patients are aware of the fact that aspirin also causes bleeding from the lower GI tract (i.e. small and large bowels).
In fact, the number of cases of aspirin-associated lower GI bleeding is rising. According to the data from the Prince of Wales Hospital (PWH), 1,800 cases of GI bleeding were managed in 2015; about 300 cases are due to bleeding from the small and large bowels, accounted for around 20% of all GI bleeding cases, the majority of which were related to aspirin. Currently, there is no effective protective treatment against the injurious effect of aspirin on the lower GI tract. Adding stomach protective drugs or switching to other non-aspirin anti-platelet drugs cannot solve this problem.
Should aspirin be continued after an episode of lower GI bleeding? To date, there is no local or international practice guideline on this. The risk of recurrent bleeding is not known if aspirin is continued. On the other hand, the risk of heart attack or stroke is also unknown if aspirin is discontinued. In clinical practice, this is a serious dilemma.
Aspirin discontinuation leads to increased risks in serious cardiovascular events
To assist physicians to better make clinical decisions for patients with high risk of cardiovascular diseases and a history of lower GI bleeding, a single-center retrospective cohort study was conducted by the Faculty of Medicine at CUHK. A cohort of patients with aspirin-associated lower GI bleeding attending PWH between 2000 and 2007 were identified and clinical data of 295 patients were analysed. Patients were divided into 2 groups (the Non-user group and Aspirin group) according to their cumulative exposure to aspirin during a 5-year period.
The results showed that among aspirin users with a history of lower GI bleeding, discontinuation of aspirin would lead to a 61% increase in serious cardiovascular events including nonfatal myocardial infarction, nonfatal stroke, or death from vascular causes, while the risk of recurrent lower GI bleeding decreased by 63%. Details are tabulated below:
|
|
% of patients with recurrent lower GI bleeding |
% of patients with serious cardiovascular events |
|
Aspirin group |
19% |
23% |
|
Non-user group |
7% |
37% |
|
Risk of Non-user group compared with Aspirin group |
Decreased by 63% |
Increased by 61% |
Benefits and risks of resuming aspirin should be carefully weighed
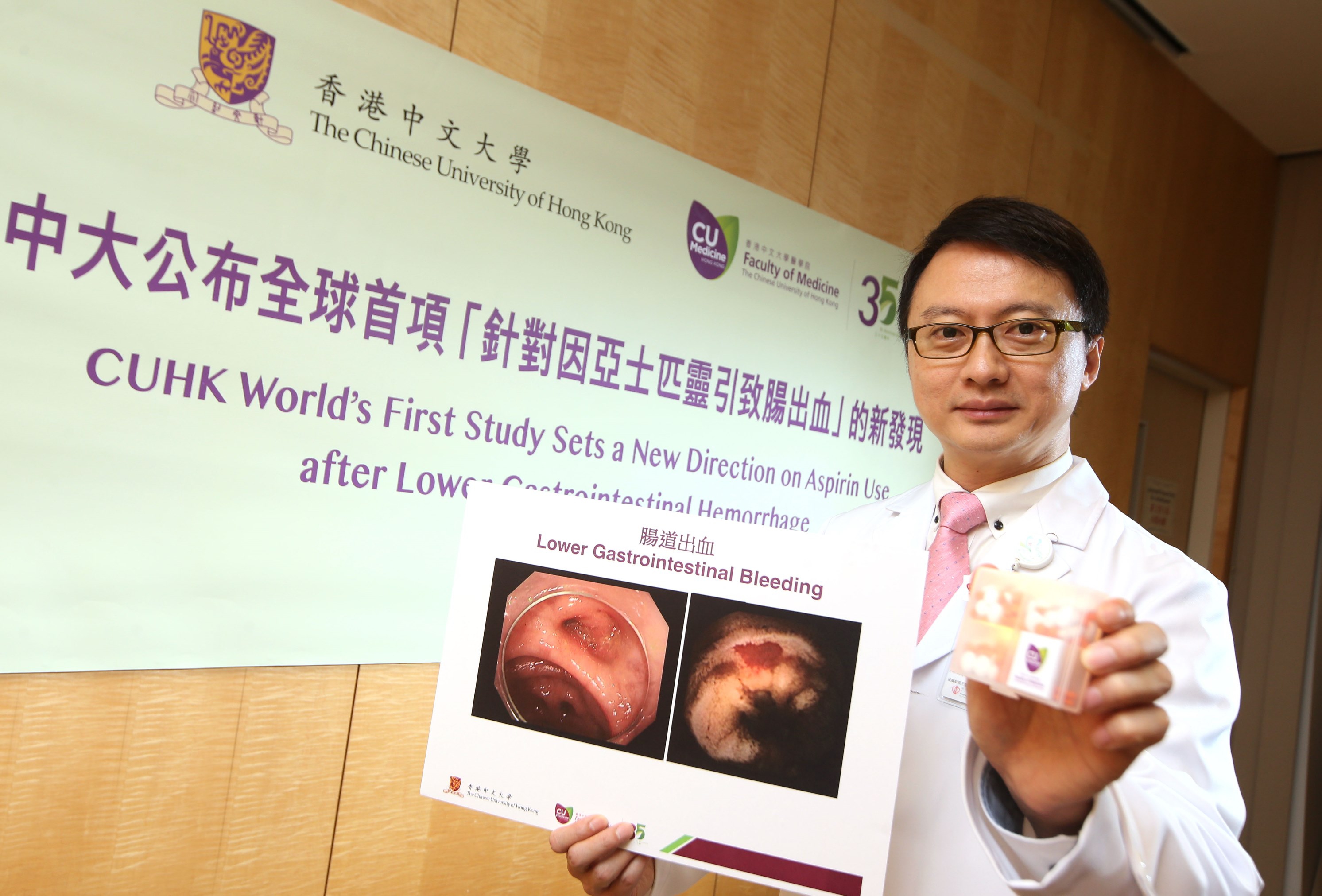
The principal investigator of the study, Prof. Francis Ka Leung CHAN, Dean of the Faculty of Medicine and Choh-Ming Li Professor of Medicine and Therapeutics at CUHK said that physicians should critically evaluate individual patients’ cardiovascular risk before discontinuing aspirin therapy. He suggested, ‘for patients with a history of myocardial infarction, coronary stents or stroke, the benefit of continuation of aspirin will outweigh its potential bleeding risk despite a history of lower GI bleeding. In contrast, patients who have been taking aspirin for primary prevention or trivial cardiovascular conditions should discontinue aspirin use if they experienced an episode of lower GI bleeding.’
Professor Chan added, ‘The above findings have not been previously reported in literature. The study achieves an important objective of providing a significant reference for personalized clinical care for patients with high cardiovascular risk after lower GI bleeding. It also provides new clinical data to assist physicians to communicate with patients, enhancing their understanding of the benefits and risks of aspirin therapy. The findings would be incorporated into the practice guidelines of various professional bodies in the United States.’
An accompanying editorial in the same issue of Gastroenterology contributed by Prof. Deepak L. BHATT of Harvard Medical School and Prof. Richard H. HUNT of the Division of Gastroenterology at McMaster University stated that the overall management for patients with high risk of cardiovascular diseases with lower GI bleeding history is controversial because there is a lack of references. The present study adds meaningfully to the understanding of the risks and potential benefits of the use of aspirin in these patients, which is an under-researched area.
Prof. Francis Ka Leung CHAN, Dean of the Faculty of Medicine and Choh-Ming Li Professor of Medicine and Therapeutics at CUHK, leads the world’s first study on aspirin use after lower GI bleeding.