CUHK
News Centre
CUHK research discovers cytokines activate growth of blood vessels and helps treat ischemia-induced tissue damage
– Peripheral arterial disease (PAD) and diabetes may cause complications, including damage to blood vessels and nerves.
– Cytokines IL-4 and IL-13 – small proteins in the body – can directly help restore blood flow to damaged tissues.
A group of scientists led by Professor Jack Wong Wing-tak from The Chinese University of Hong Kong (CUHK)’s School of Life Sciences has made a groundbreaking discovery about how the body creates new blood vessels in damaged tissue. The team found that certain cytokines – small proteins in the body – called IL-4 and IL-13 play a vital role in activating the growth of blood vessels in areas where blood flow is restricted. This discovery could lead to new treatments for conditions like peripheral arterial disease (PAD) and diabetes-related blood flow problems. The research has been published in the scientific journal Cell Reports.
Patients with both PAD and diabetes may suffer from higher risk of amputation
PAD is a common condition that affects millions of people worldwide, especially the elderly. It narrows or blocks vessels that carry blood from the heart to the legs. When a person has both PAD and diabetes, it causes various complications, including damage to blood vessels and nerves, with the combination of reduced blood flow from blocked arteries and the already weakened blood vessels from diabetes creating a difficult situation.
The compromised blood vessels, along with poor circulation and impaired wound healing, make it difficult for oxygen and nutrients to reach the legs, resulting in tissue damage. If left untreated, severe tissue damage can lead to non-viable tissue, infections and the need for amputation to prevent further complications.
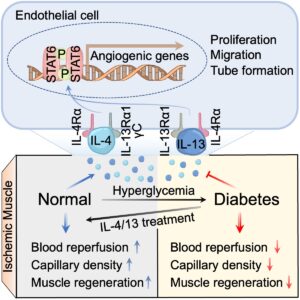
Cytokines IL-4 and IL-13 restore blood flow to damaged tissue by acting on endothelial cells
Endothelial cells are the cells that line the inside of blood vessels, and they play a crucial role in the process of creating new blood vessels. They receive signals from the blood-restricted environment and then go through a series of intricate steps, such as growing in number, moving to the right places and forming tube-like structures, to create new blood vessels. These new blood vessels branch out from the existing ones and extend towards the blood-restricted area. However, scientists still don’t fully understand how the immune system and endothelial cells work together to restore blood flow to damaged tissue.
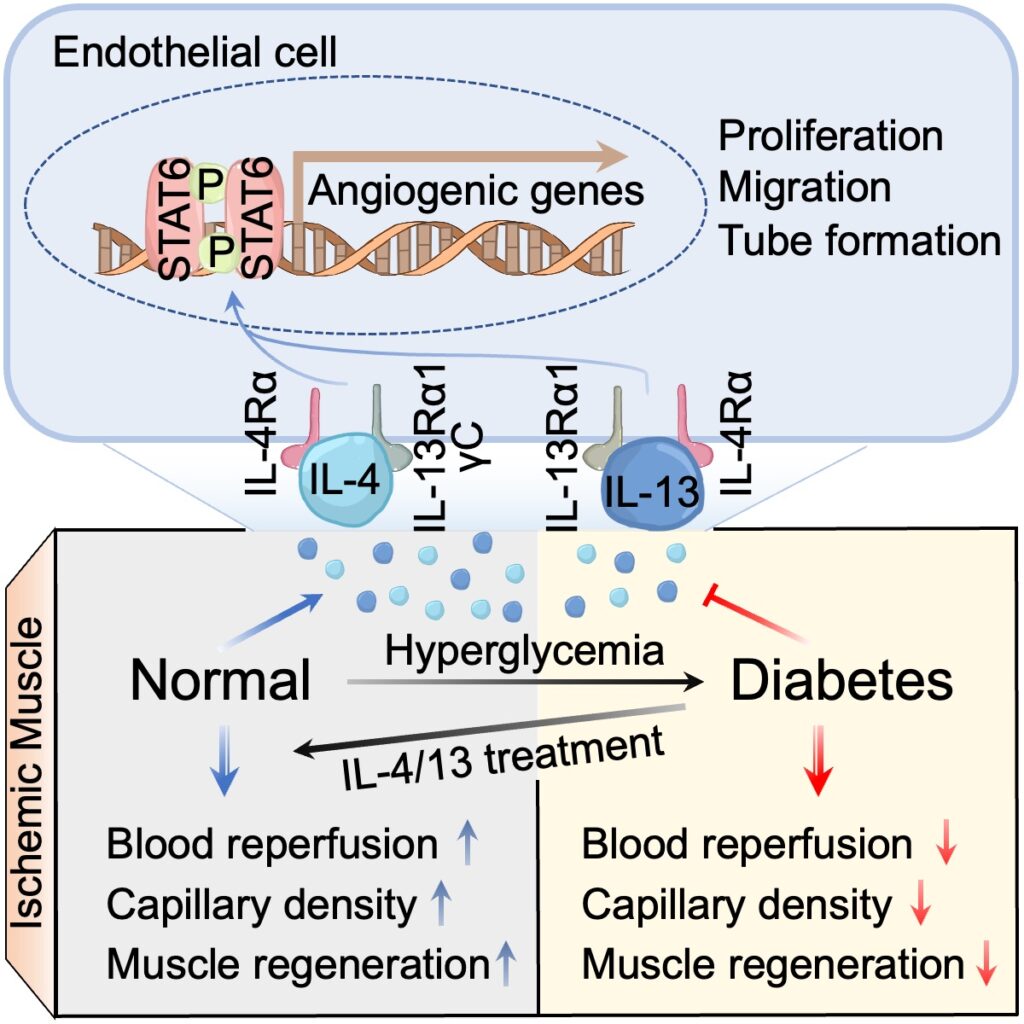
Previous studies have shown that certain cytokines, called IL-4 and IL-13, are crucial mediators of the immune response. They help keep body tissues healthy by changing a type of immune cell called macrophages to make repairs to damage caused by various medical conditions, such as heart attack, stroke and kidney injuries. However, in the context of leg ischemia, Professor Wong’s team found that instead of working via macrophages, IL-4 and IL-13 can directly help restore blood flow to damaged tissue by acting on another type of cell called endothelial cells, which are not immune cells. These cytokines have been found to stimulate endothelial cells to grow, move and form new blood vessels. By harnessing these activities, substances like IL-4 and IL-13 can enhance the growth of new blood vessels, improving blood flow and promoting tissue regeneration.
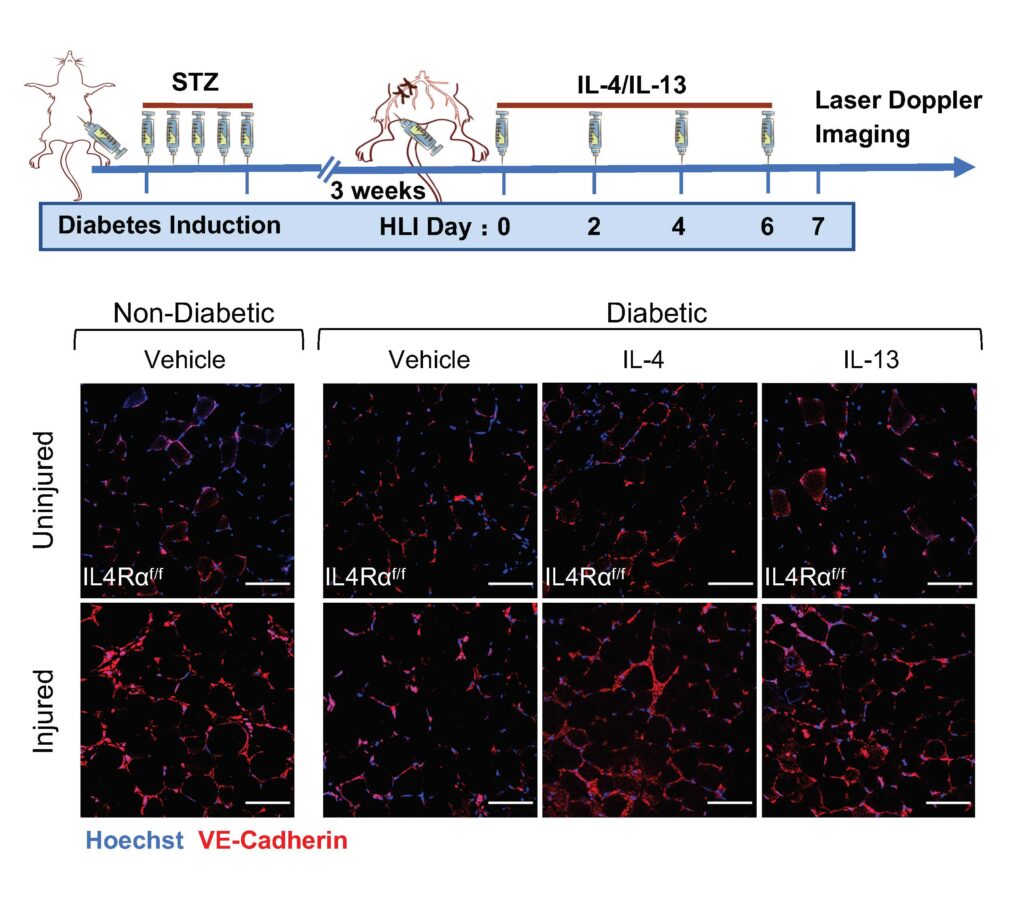
“Diabetes mellitus is a major risk factor for PAD and can worsen its progression and increase mortality,” explained Professor Wong. “Our team also found that low levels of IL-4 and IL-13 may be one reason why people with diabetes have difficulty healing damaged tissue. We discovered that treating diabetic mice with IL-4 and IL-13 helped restore blood flow and promote tissue regeneration. This research is an important step forward in understanding how the body repairs damaged tissue and how we can develop new treatments for PAD and related conditions.”
The research team envisions collaborating with medical units to conduct clinical trials evaluating the efficacy and safety of IL-4 and IL-13 as therapeutic agents. The team also plans to explore combination therapies involving IL-4 and IL-13 in conjunction with existing treatments. By advancing understanding and exploring these potential developments, the team aspires to enhance patient care for people with these conditions.

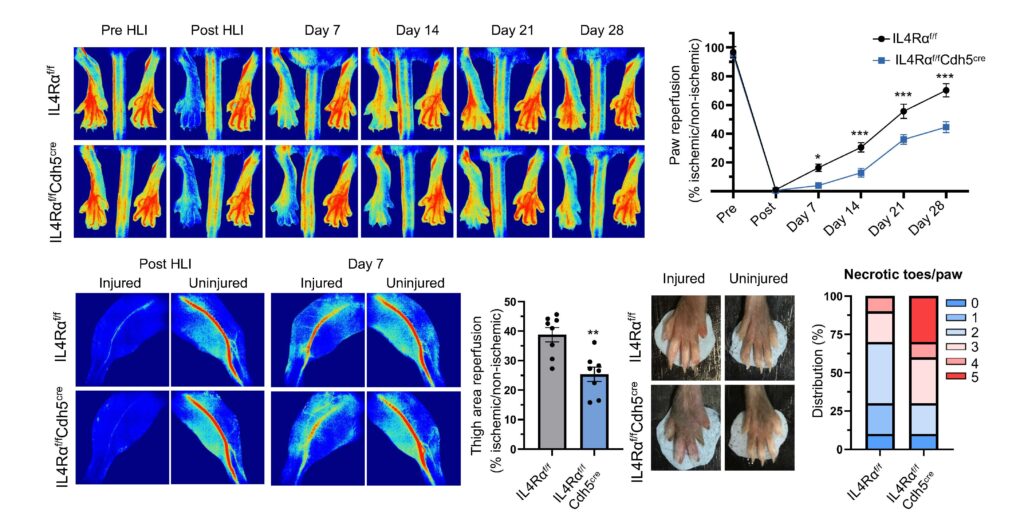
The restoration of blood flow in the limbs of mice with and without a specific receptor (IL4Rα) in endothelial cells.