CUHK
News Centre
CUHK identifies Streptococcus anginosus as a pathogen that promotes gastric tumour formation
The Chinese University of Hong Kong (CUHK)’s Faculty of Medicine (CU Medicine)’s latest study has identified Streptococcus anginosus (S. anginosus), a non-Helicobacter pylori (H. pylori) bacterium, as a pathogen of gastric cancer. Professor Yu Jun and her research team discovered that S. anginosus was enriched in the gastric mucosa of patients with gastric cancer. After further investigation in mice, the team confirmed the bacterium induces inflammation and atrophy in the stomach and accelerates carcinogenesis. They have also unravelled the mechanism of its colonisation of the stomach, which will provide new insights for clinical intervention in the future. Findings of this study have been published in Cell, one of world’s top biology journals; and this is the first study led by CUHK investigators to be published in it.
S. anginosus is commonly found in the oral cavity
Gastric cancer is the fifth most common cancer worldwide and sixth in Hong Kong. Though H. pylori infection is known to be a major risk factor for gastric cancer, only 1%-3% of infected individuals eventually develop the disease. Whether other microorganisms beyond H. pylori are involved in gastric carcer formation remains unknown.
A CU Medicine research team therefore explored the non-H. pylori gastric microbiome in patients with different stages of gastric tumourigenesis, from superficial gastritis, atrophic gastritis and intestinal metaplasia to cancer. They discovered five oral pathogens that were enriched in patients’ gastric mucosa, including S. anginosus, a kind of bacteria commonly found in the oral cavity, nasopharynx, gastrointestinal tract and vaginal tract. It is an opportunistic pathogen and may cause invasive infections after entering sterile sites in the body, including oral and non-oral ones. Due to its resilience to low pH conditions, S. anginosus can survive in and colonise the gastric mucosa. Data from research team’s laboratory showed S. anginosus infection is very common that it can be found in the gastric mucosa of 50%-70% of the Chinese subjects while the infection rate of H. pylori is about 40%.
S. anginosus induces acute gastric inflammation and promotes carcinogenesis over a period of time
The researchers further studied how S. anginosus induces inflammation and leads to carcinogenesis using mice models. They found that S. anginosus infection rapidly induced acute gastritis in mice, and consequently turned into chronic gastritis, gastric mucinous metaplasia and dysplasia over a long period of time.
The mechanism behind S. anginosus-related gastric carcinogenesis
The research team has further established the mechanism by which S. anginosus communicates with gastric epithelial cells to drive carcinogenesis. The bacterium colonises gastric cells through its surface protein TMPC directly binding to gastric cells’ receptor protein ANXA2, which triggers oncogenic MAPK signalling to promote gastric cancer progression.
Professor Yu Jun, corresponding author of this paper, Choh-Ming Li Professor of Medicine and Therapeutics, director of State Key Laboratory of Digestive Disease (CUHK) and director of Institute of Digestive Disease at CUHK, said, “We first analysed data from different human cohorts and found that S. anginosus abundance was associated with atrophic gastritis, intestinal metaplasia and gastric cancer. We have established the role of S. anginosus in gastric carcinogenesis and its related mechanism; next we will explore the therapeutic potential of targeting it to reduce gastric inflammation and cancer risk.”
She added, “We spent five years to complete this study and we are extremely grateful to have it accepted and published in Cell, one of world’s most prestigious journals. It feels like conquering Mount Everest, as the journal is known for its stringent requirements in novelty and comprehensiveness.”
Professor Joseph Sung Jao-yiu, co-corresponding author of this paper, CUHK Emeritus Professor of Medicine, Dean of Lee Kong Chian School of Medicine, and Senior Vice President (Health and Life Sciences) at Nanyang Technological University, Singapore, remarked, “H. pylori infection and family history are widely recognised as the two main risk factors for gastric cancer. The discovery of enrichment of S. anginosus in the gastric mucosa across different stages of gastric cancer opens up a whole new direction in understanding the pathogenesis of gastric cancer. We also wish to flag that co-infection of H. pylori and S. anginosus leads to an even higher risk of precancerous atrophy, metaplasia, or gastric cancer.”
Dr Fu Kaili, first author of the study, PhD student and now post-doctoral fellow in the Department of Medicine and Therapeutics at CU Medicine, said, “Our investigation revealed that S. anginosus has a causal relationship with gastric cancer and that it promotes carcinogenesis in a gastritis and precancerous atrophy-metaplasia-dysplasia sequence. We also found that S. anginosus impairs gastric barrier function and promotes cell proliferation, altering the gastric microbiome to a more favourable environment for cancer progression.”

CU Medicine’s latest study has identified Streptococcus anginosus (S. anginosus), a non-Helicobacter pylori (H. pylori) bacterium, as a pathogen of gastric cancer. Research team discovered that S. anginosus was enriched in the gastric mucosa of patients with gastric cancer and unravelled the mechanism of its colonisation of the stomach. Findings of this study have been published in Cell, one of world’s top biology journals; and this is the first study led by CUHK investigators to be published in it.
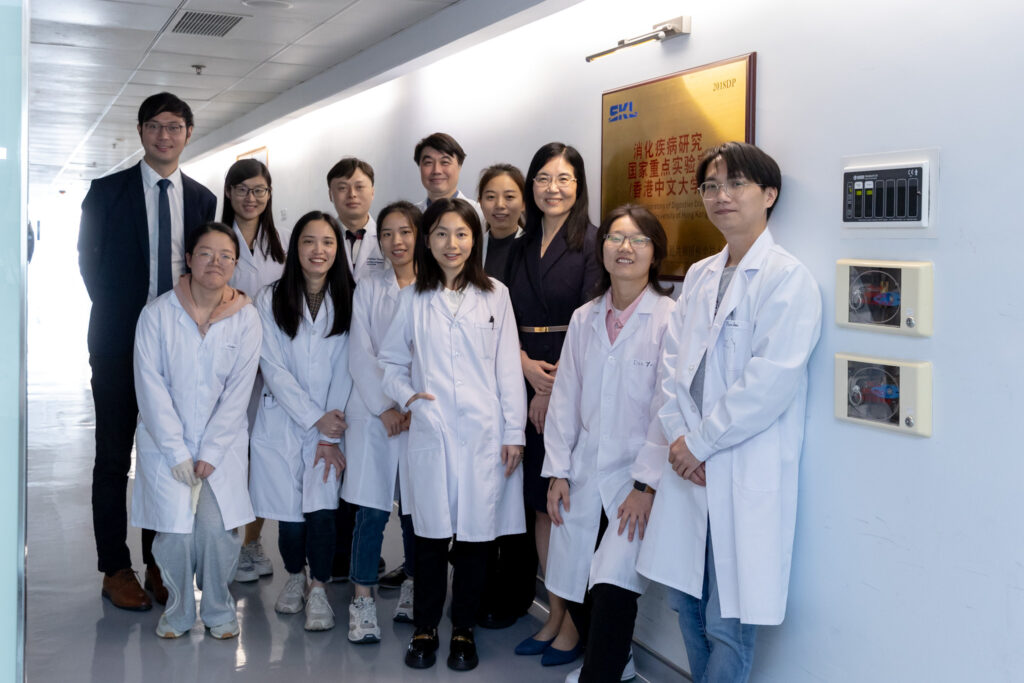
(From left) Professor Joseph Sung Jao-yiu, CUHK Emeritus Professor of Medicine, Dean of Lee Kong Chian School of Medicine, and Senior Vice President (Health and Life Sciences) at Nanyang Technological University, Singapore; Professor Yu Jun, Choh-Ming Li Professor of Medicine and Therapeutics, director of State Key Laboratory of Digestive Disease (CUHK) and director of Institute of Digestive Disease at CUHK; and Dr Fu Kaili, PhD student and now post-doctoral fellow in the Department of Medicine and Therapeutics at CU Medicine.

Dr Fu Kaili says S. anginosus impairs gastric barrier function and promotes cell proliferation, altering the gastric microbiome to a more favourable environment for cancer progression.

Professor Joseph Sung Jao-yiu points out that co-infection of H. pylori and S. anginosus leads to an even higher risk of precancerous atrophy, metaplasia, or gastric cancer. He reminds the public to take good care of oral hygiene to avoid diseases that enter by the mouth.