CUHK
News Centre
CUHK-HKU Study on Multi-gene Mutation-Drug Matching for Recurrent Ovarian Cancer Patients Providing Free Pharmacogenomic Analysis for 100 Patients in Hong Kong
The Faculty of Medicine of The Chinese University of Hong Kong (CUHK) and the Li Ka Shing Faculty of Medicine of The University of Hong Kong (HKU) are going to launch the city’s first collaborative study with the aim of providing expert affordable multi-gene mutation – drug matching for recurrent ovarian cancer patients. The research goal is to help identify a more precise choice of drug, based on tumour DNA characteristics using modern pharmacogenomic analysis. At the same time, the research team will determine the prevalence of potential druggable DNA events in Asian recurrent ovarian cancer patients. This Hong Kong Cancer Fund-sponsored study will provide free analysis for 100 local patients.
Ovarian cancer recurrence can be up to 80% in late stage with no precise regimen
According to the data of the Hong Kong Cancer Registry 2015, ovarian cancer is the 6th most common cancer type for Hong Kong females, with an average of over 500 new cases each year, and ranks 7th in overall cancer mortality rates. There is also an increasing trend in its incidence since the 1980s. The causes of ovarian cancer are still uncertain and early symptoms are not obvious. 34% of patients are in stage III or IV at the time of diagnosis. Standard treatment of ovarian cancer is surgery with proper staging. In late stage cancer, removal of all gross tumours is the goal. However, for these advanced stage patients, despite such radical treatment, recurrence is common and can be up to 80%. In the majority of recurrent cases, surgery is not suitable and chemotherapy is the mainstay of treatment.
Prof. Hextan Yuen-Sheung NGAN, Tsao Yin-Kai Professor in Obstetrics and Gynaecology, Chair Professor and Head of the Department of Obstetrics and Gynaecology, Li Ka Shing Faculty of Medicine, HKU said, ‘The response rate of the drug treatment for recurrent patients varies from 20 – 40%. Though we have quite a number of drugs that can be used to treat recurrent ovarian tumour, we do not know which one has the best response. We therefore need a more precise way of choosing the most effective regimen.’
Study aims at helping recurrent ovarian cancer patients to find a drug option based on DNA sequencing multiple genes
Pharmacogenomic analysis can help identify a more precise choice of drug based on tumour DNA characteristics. The analysis first requires tumour DNA to be sequenced for multiple genes which are known to be related to drug responses, followed by professional gene mutation – drug matching.
In the past, pharmacogenomic analysis was usually done for one gene at a time (e.g. EGFR mutation for lung cancer to be matched for EGFR inhibitor). In the last 3 to 5 years, DNA sequencing technology has become more mature and professional gene mutation – drug matching expertise is available in Hong Kong.
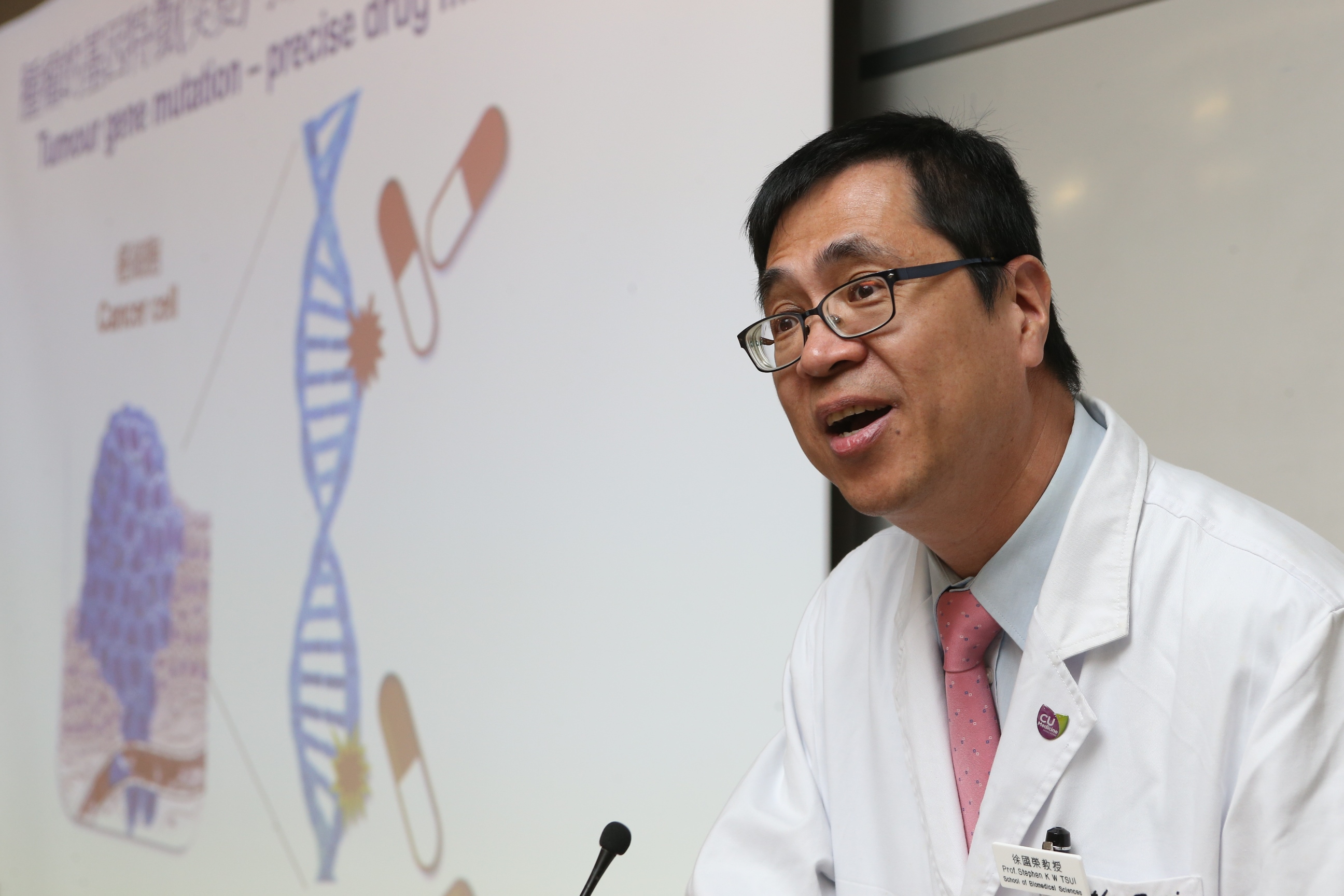
Prof. Stephen Kwok-Wing TSUI, Professor, School of Biomedical Sciences, Faculty of Medicine, CUHK said, ‘The DNA sequencing technology at CUHK, namely the Next-Generation Sequencing (NGS), can simultaneously sequence multiple genes, hundreds or tens of thousands of genes, in a few hours, which would have taken several months to a year in the past. The advanced technology allows us to perform multi-gene sequencing very quickly and accurately, taking very small amounts of tumour DNA samples (nanograms).’
CUHK has established a responder gene-drug database from over 150 clinical studies of ovarian cancers and additional cancers
The CUHK team has established the Responder Gene Panel from the results of over 150 clinical studies of ovarian cancer and additional cancer types from more than 18 countries in the US, Europe and Asia. It is designed to enable pharmacogenomic analysis of patient tumour samples using the NGS technology in Hong Kong. Along with expert drug matching, the Responder Gene Panel can reliably tell the presence or absence of drug-associated gene mutations in a patient’s tumour, which can serve to identify potential drug options for patients based on tumour DNA evidence.
The Panel includes all reported ovarian cancer patient DNA mutations that are associated with good and exceptional clinical responses to specific drug treatments, as of 2017. It is estimated that about 30% (or more) of ovarian cancer patients may have these ovarian responder mutations. Any enrolled ovarian cancer patient whose tumours carry these responder DNA mutations will receive a DNA-drug matching research result as genetic evidence and as a reference for drug choice by the patient’s physician-in-charge. The patients can also choose to receive any information associated with additional cancer types as an additional record.
Prof. Vivian Wai Yan LUI, Associate Professor, School of Biomedical Sciences, Faculty of Medicine, CUHK, an expert in cancer pharmacogenomics said, ‘A similar approach has been widely adopted in more advanced countries such as the US. Our goal is to promote the use of multi-gene pharmacogenomics analysis in Hong Kong ovarian cancer patients to help identify tumour DNA events that may guide precise drug choice quickly. At the same time, we can determine the frequency of occurrence of these potential druggable DNA events in Asian ovarian cancer patients. Our study comprises a team of experts from Hong Kong, the US, and the UK on cancer, precision medicine and medication. The study will also follow-up on patients for up to 2 years to investigate the feasibility of pharmacogenomics in Hong Kong.’
The study is sponsored by Hong Kong Cancer Fund. It will officially start on 8 December this year, with the target of recruiting 100 patients in Hong Kong over the next 16 months. Interested patients can call 3943-5382 or email to ovcamut@cuhk.edu.hk. For details, please refer to the project website: http://cuhk.edu.hk/proj/ovcamut/
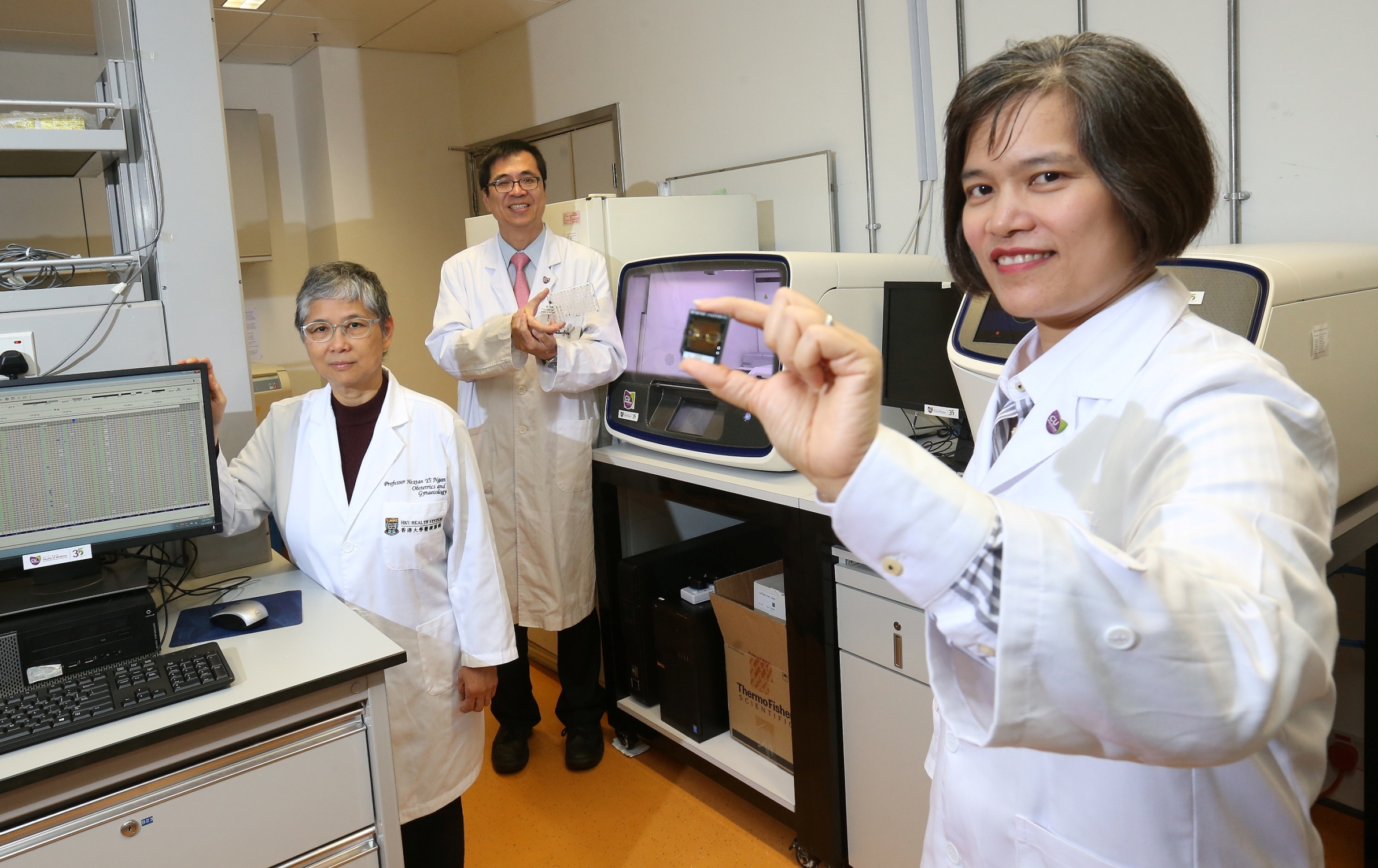
The Faculty of Medicine of CUHK and the Li Ka Shing Faculty of Medicine of HKU are going to launch the city’s first collaborative study with the aim of providing expert affordable multi-gene mutation – drug matching for recurrent ovarian cancer patients. From left: Prof. Hextan Yuen-Sheung NGAN, Tsao Yin-Kai Professor in Obstetrics and Gynaecology, Chair Professor and Head of the Department of Obstetrics and Gynaecology, Li Ka Shing Faculty of Medicine, HKU; Prof. Stephen Kwok-Wing TSUI, Professor, School of Biomedical Sciences, Faculty of Medicine, CUHK; and Prof. Vivian Wai Yan LUI, Associate Professor, School of Biomedical Sciences, Faculty of Medicine, CUHK.
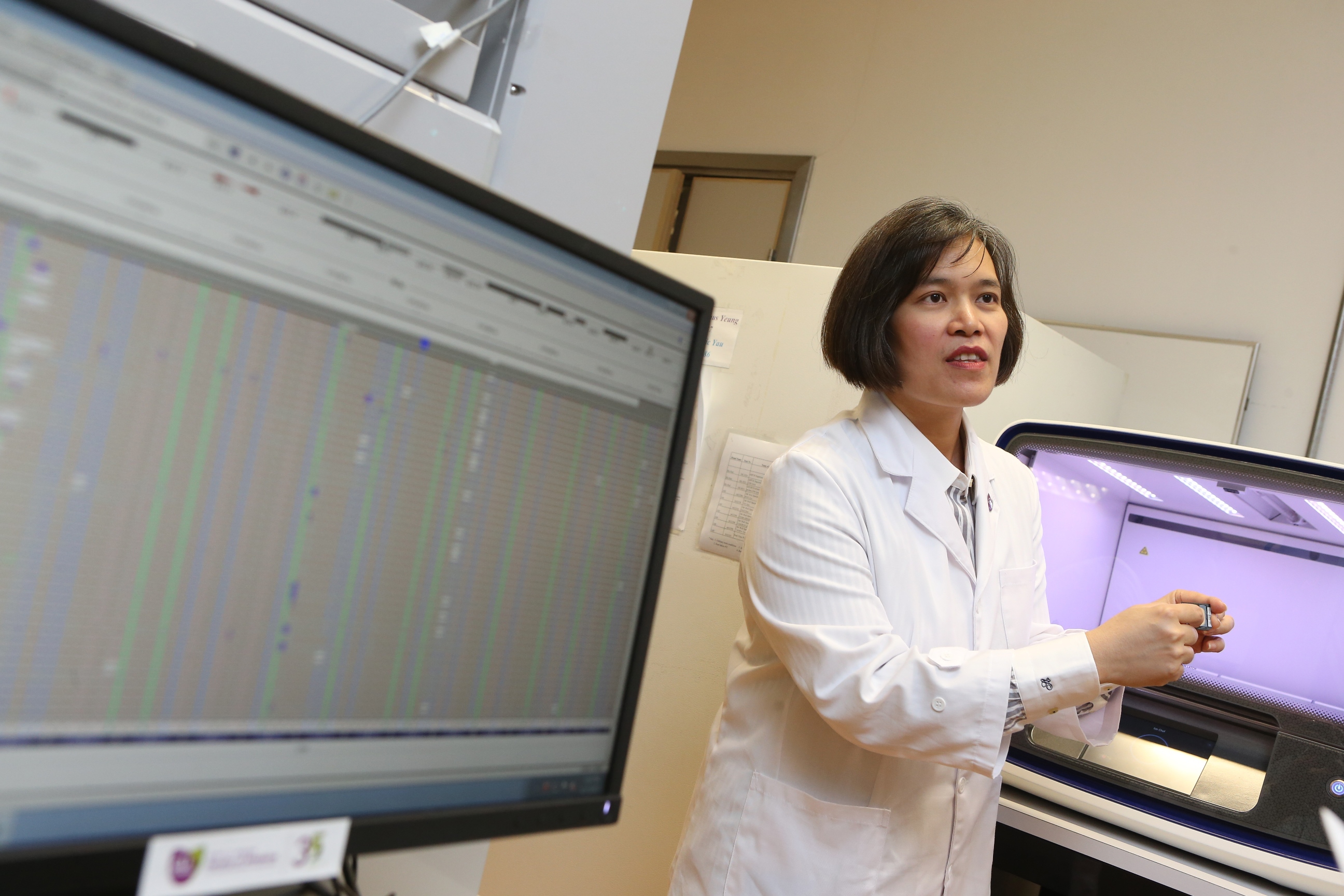
Professor LUI wants to promote the use of multi-gene pharmacogenomics analysis in Hong Kong ovarian cancer patients to help identify tumour DNA events that may guide precise drug choice quickly.
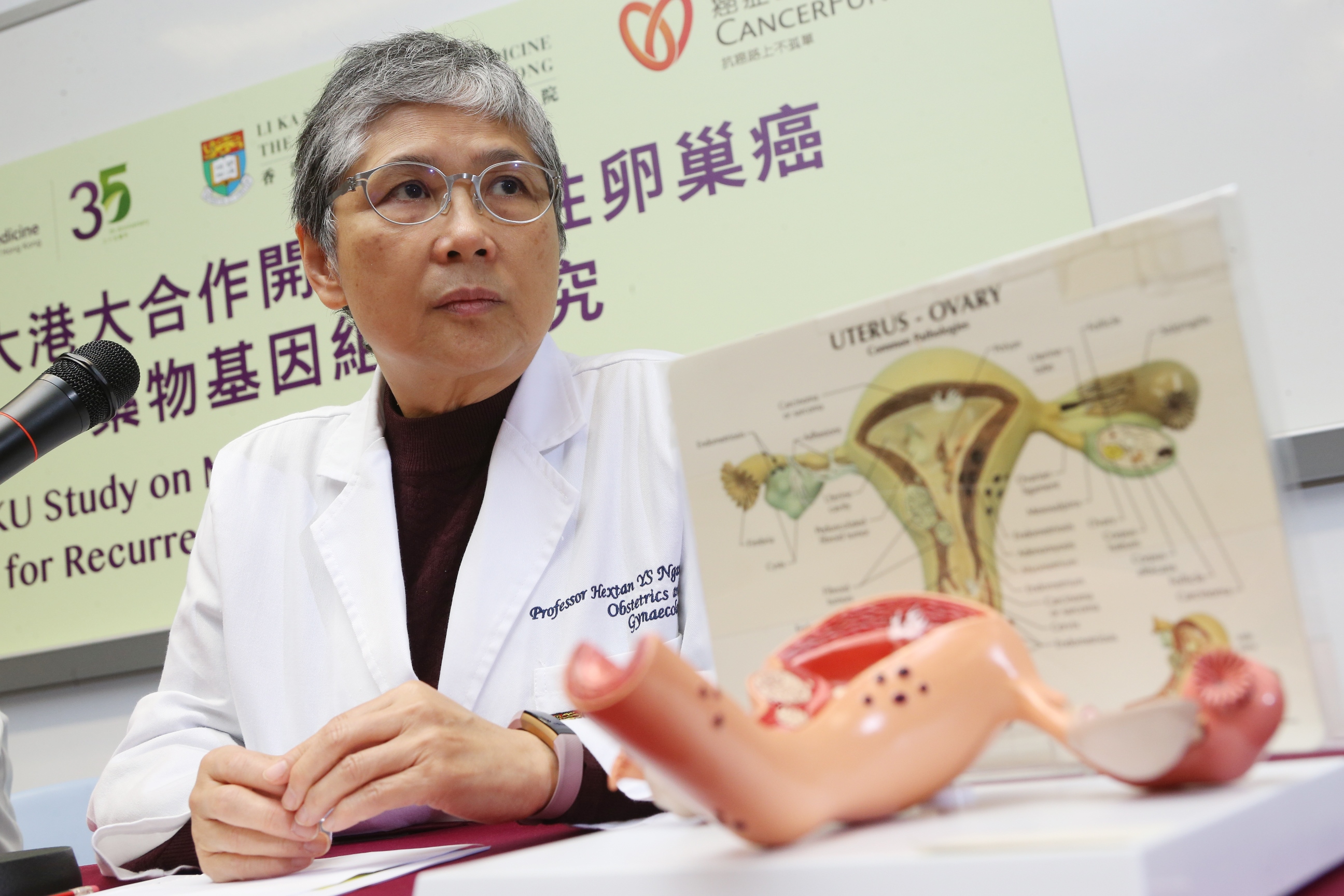
Professor NGAN says despite removal of all gross tumours, ovarian cancer recurrence can be up to 80% in late stage and therefore precise regimen is needed.