CUHK
News Centre
CUHK discovers a blood regulator linked to tumour microenvironment formation, sparking a new therapeutic target for lung cancer
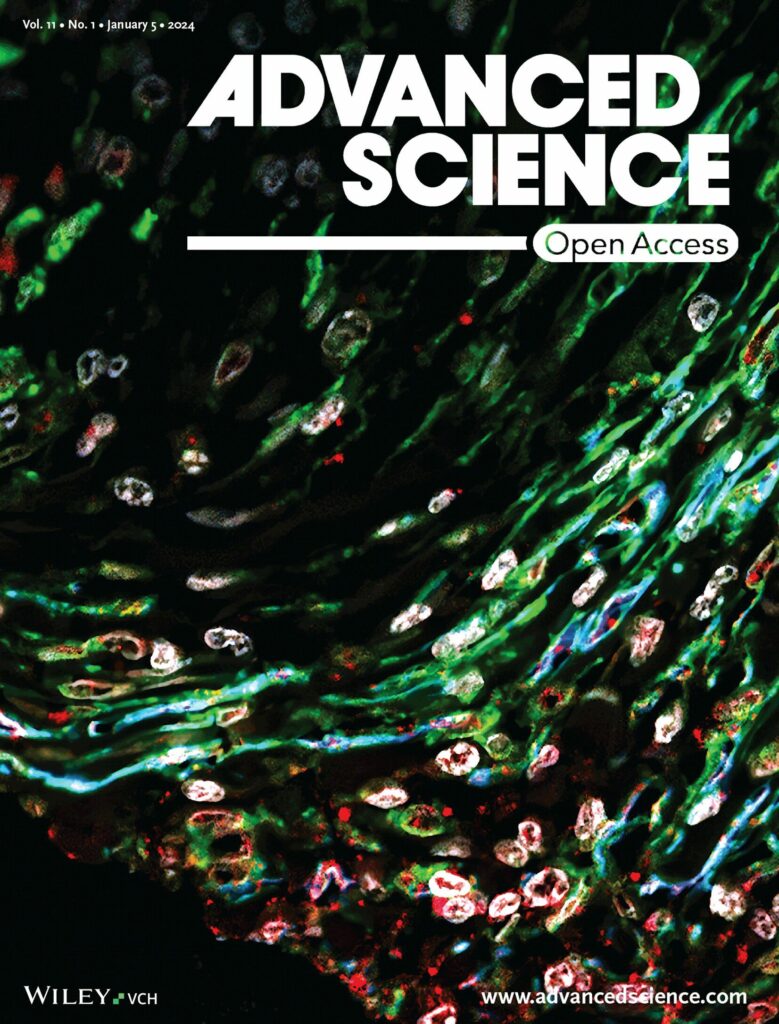
Lung cancer is the leading cause of cancer deaths in Hong Kong and worldwide, but there is still an unmet clinical need for effective therapeutic strategies. A new study from The Chinese University of Hong Kong (CUHK)’s Faculty of Medicine (CU Medicine) has discovered that lung cancer can utilise a blood formation regulator to construct the tumour microenvironment. The team validated the translational potential and safety of this new target on experimental models, demonstrating its clinical relevance for lung cancer. The findings have been published in the leading international scientific journal Advanced Science.
Seeking new hope for lung cancer treatment from the tumour microenvironment
Cancer cells are heterogeneous and therefore difficult to eliminate completely. Effective cancer treatment remains a major clinical challenge.
Professor Patrick Tang Ming-kuen, Assistant Professor in the Department of Anatomical and Cellular Pathology at CU Medicine, said, “Increasing evidence demonstrates that the tumour microenvironment – that is, non-cancerous cells in tumour tissue – is important for cancer growth and metastasis. In contrast to cancer cells, the tumour microenvironment is not heterogeneous, making it an ideal target for cancer therapy. Nowadays, advances in single-cell bioinformatics allow us to better understand the tumour microenvironment, so that some cancer-promoting mechanisms that can only be observed at the single-cell level can be discovered, which may be useful for cancer treatment.”
In 2022, the same team reported an important phenomenon “Macrophage-Myofibroblast Transition” (MMT) for the formation of the tumour microenvironment. This mechanism causes macrophages, anti-cancer immune cells, to be further transformed into cancer-promoting myofibroblasts in lung cancer due to long-term overactivation. The underlying mechanism is still largely unclear.
Dr Philip Tang Chiu-tsun, Postdoctoral Fellow in the Department of Anatomical and Cellular Pathology at CU Medicine, explained, “Here, we attempted to investigate the underlying regulation at the single cell level and unexpectedly discovered that a hematopoietic regulatory factor, Runx1 (full name Runt-related transcription factor 1) is critical for promoting patients’ macrophages undergoing MMT, which may represent an effective target for lung cancer treatment.”
Clinical significance of Runx1 as a redundant hematopoietic pathway in cancer therapy
Professor Patrick Tang commented, “Since Runx1 plays an important role in blood formation, inhibiting Runx1 may affect hematopoietic function, leading to doubts about its clinical value in cancer treatment. Fortunately, a new study (Blood Adv (2021) 5 (23): 4949–4962) showed that zebrafish lacking Runx1 can still maintain normal haematopoiesis through other pathways.” Mr Max Chan Kam-kwan, PhD student in the same department, added, “Encouragingly, genetic and pharmaceutical inhibition of Runx1 effectively inhibited MMT and tumour growth in mice, and no side effects were detected.”
Professor To Ka-fai, Professor in the Department of Anatomical and Cellular Pathology, highlighted the clinical importance of this study. “The preclinical data generated from this work will serve as an important rationale for further transforming tumour microenvironment discoveries into clinical applications. It may eventually develop into an effective solution to end cancer via targeting MMT.”
This study was supported by the Research Grants Council of Hong Kong, the Health and Medical Research Fund, the State Key Laboratory of Translational Oncology, and CU Medicine’s Passion for Perfection scheme and Faculty Innovation Award. Other key participants in the study included Professors Calvin Ng Sze-hang, Leung Kam-tong and Lan Hui-yao from CU Medicine.
The original study can be accessed here: https://onlinelibrary.wiley.com/doi/10.1002/advs.202470006