CUHK
News Centre
CU Medicine Study Proves Pocket-size Mobile Echocardiographic Screening Device Effective in Detecting Thoracic Aortic Aneurysm
Thoracic aortic aneurysm (TAA) is common among hypertension patients and is one of the top leading causes of death in Hong Kong. TAA is a potentially life-threatening condition with catastrophic complications including aortic dissection and rupture. A latest study from the Faculty of Medicine at The Chinese University of Hong Kong (CU Medicine) proved that a pocket-size mobile echocardiographic device (PME device) is effective in detecting TAA in an outpatient setting, with a true positive value of 92%. With the PME device, the research team conducted the world’s largest reported TAA screening study for patients with a history of hypertension. It found the prevalence of TAA among this subject population was 7.5% and identified male gender and older age as independent factors associated with the disease. The findings have been published in an international journal The Annals of Thoracic Surgery.
TAA accounts for 300 deaths every year in Hong Kong
TAA is the second most common aorta disease after atherosclerosis worldwide. It accounts for more than 1,400 hospital admissions and 300 deaths every year in Hong Kong. The disease was defined as a permanent dilation of the aorta with a > 50% increase in diameter relative to the diameter of the adjacent normal segment or with a diameter of ≥ 4.5 cm.
Dr. Randolph Hung Leung WONG, Clinical Associate Professor (honorary), Division of Cardiothoracic Surgery, Department of Surgery, CU Medicine explained, “TAA happens when an aorta in the chest is weakened. When the aorta is weak, blood pushing against the vessel wall can cause it to bulge like a balloon and becomes aneurysm. Complications such as aorta dissection and rupture can result in life-threatening bleeding or sudden death and surgeries under these conditions are extremely challenging and associated with high risks. Aortic aneurysm is a silent killer as 95% of cases carry no symptoms. Our unit is seeing an increase in the number of aortic related diseases from around 20 cases 10 years ago to currently around 90 cases per year. The important risk factors for TAA include high blood pressure, old age, being male, smoking, and use of medications that may affect immunity.”
PME device promotes more accessible TAA initial screening
Due to the absence of clinical symptoms or signs, TAA cannot be easily detected by conventional physical examinations. Computed tomography (CT) scan with contrast in the chest has been considered the gold standard diagnostic confirmatory test for TAA.
Professor Simon Chun Ho YU, Chairman of Department of Imaging and Interventional Radiology at CU Medicine said, “Though Contrast CT is the gold standard in the diagnosis of TAA, it has its disadvantages — irradiation hazard, nephrotoxic contrast and high cost. Transthoracic echocardiography is a reasonably acceptable imaging test (about 90% accuracy) for the initial screening of TAA. Previous studies have shown PME devices can provide point-of-care aortic ultrasound with high sensitivity (ranging from 81% to 100%) and specificity for detecting anatomic cardiac structures (ranging from 68% to 100%) as compared to transthoracic echocardiography. In 2011, the European Association of Echocardiography approved the use of PME devices in screening programmes. We believe it is important to detect asymptomatic TAA patients earlier to allow us to monitor them closer and offer timely surgical intervention before devastating complications of aortic dissection or rupture.”
Study showed prevalence of TAA among Chinese hypertensive population is high
The CU Medicine research team recruited 1,529 Chinese hypertensive patients with a mean age of 62, who attended their hypertension clinics between June 2016 and July 2018, for a transthoracic aortic ultrasound using a point-of-care PME device. The echo examinations obtained aortic diameter measurements including the aortic sinus, sinotubular junction, ascending aorta, aortic arch, and descending thoracic aorta through various standard echo views. The team analysed the data and came up with the following findings:
- The prevalence of TAA in the study population was 7.5% (115/ 1,529).
- Of the 115 patients with TAA, 64 patients were with aortic diameter ≥ 4.5 cm, 73 were with > 50% localised increase in diameter compared with adjacent normal segment, and 22 were with both conditions.
- Patients with TAA were significantly older and more likely to be men. More than half of the affected population are elderly people aged between 65 and 85 years.
- The aortic arch and distal ascending aorta were found to be the most commonly affected segments, followed by the aortic sinus.
- Among 38 patients with aortic diameter ≥ 4.5 cm who received further contrast CT assessment, 35 were confirmed of aneurysm, giving a true positive value of 92.1% for PME devices in TAA detection.
Professor Alex Pui Wai LEE from the Division of Cardiology, Department of Medicine and Therapeutics at CU Medicine remarked, “Our study proved silent TAA is common among hypertensive patients in Hong Kong and we confirmed it is highly feasible to use a PME device in a clinic setting for point-of-care screening of asymptomatic hypertensive patients. A complete PME examination of all segments of the aorta only took about 10 minutes per case. After finishing a tutorial of 30 minutes, plus supervised scanning for around 20 to 30 cases, a doctor can be ready to perform the examination on patients in a clinic setting. We believe this approach will be useful for early detection of TAA among at-risk patients, allowing aggressive blood pressure control and early surgical intervention.”
Professor Martin Chi Sang WONG from The Jockey Club School of Public Health and Primary Care of CU Medicine reminded the general public to be more aware of hypertension. He said, “From academic literature, we witness an increasing number of new cases of TAA around the world. One of the most common risk factors is high blood pressure — the higher the blood pressure and the longer it goes uncontrolled, the higher the chance and seriousness of complications. Therefore, we highly recommend people to have regular check ups on blood pressure, which should start at the age of 18 years for at least once every two years. Also, adopting a healthy lifestyle is essential for preventing and controlling hypertension.”
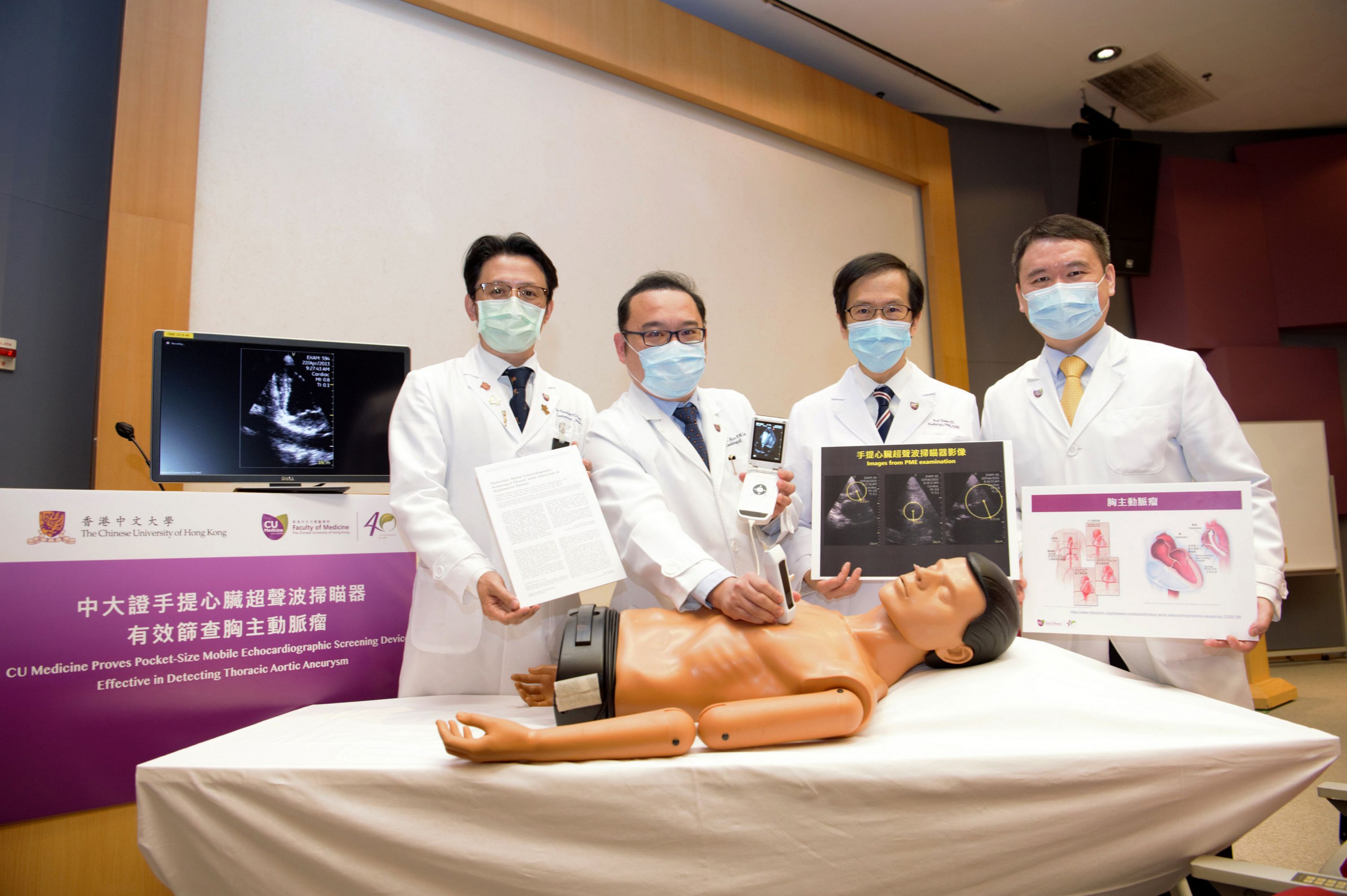
CU Medicine proves that a pocket-size mobile echocardiographic device is effective in detecting TAA in an outpatient setting. It also finds the prevalence of TAA among patients with a history of hypertension was 7.5%. (From left) Dr. Randolph Hung Leung WONG, Clinical Associate Professor (honorary), Division of Cardiothoracic Surgery, Department of Surgery; Professor Alex Pui Wai LEE from the Division of Cardiology, Department of Medicine and Therapeutics; Professor Simon Chun Ho YU, Chairman of Department of Imaging and Interventional Radiology; and Professor Martin Chi Sang WONG from The Jockey Club School of Public Health and Primary Care at CU Medicine.
Dr. Randolph Hung Leung WONG says aortic aneurysm is a silent killer as 95% of cases carry no symptoms. Complications such as aorta dissection and rupture can result in life-threatening bleeding or sudden death.
Professor Simon Chun Ho YU says PME device is convenient for point-of-care setting and with a much lower cost compared with CT scan or traditional transthoracic echocardiography. It is ideal for screening TAA patients and allows early intervention.
Professor Alex Pui Wai LEE says the PME device is as handy as doctors’ stethoscope, meaning that they can carry out scanning for patients anytime, anywhere.