CUHK
News Centre
CU Medicine is a pioneer in Asia, introducing upper airway stimulation for obstructive sleep apnoea patients
Continuous positive airway pressure treatment is effective for patients with moderate-to-severe obstructive sleep apnoea (OSA), but it has to be used every night and is not curative, resulting in low compliance. Upper airway stimulation (UAS) is an emerging surgical procedure for patients who have problems accepting or adhering to standard continuous positive airway pressure treatment.
Though UAS attained approval from The United States Food and Drug Administration in 2014 to treat OSA patients, it has remained a relatively rare treatment option in Asia. The Chinese University of Hong Kong (CUHK)’s Faculty of Medicine (CU Medicine) introduced this surgical innovation to patients in February 2023, making Hong Kong the third location in Asia to do so, after Singapore and Japan. The CU Medicine research team have completed three cases as of today, successfully improving the patients’ condition.
Upper airway stimulation provides a solution to difficulties with compliance with standard OSA treatment
OSA is a common form of sleep-disordered breathing. Patients’ upper airway muscle tone relaxes when sleeping and the upper airway is blocked. This leads to a reduction in blood oxygen levels, causing sleep fragmentation, disabling daytime sleepiness and impairing cognitive function. Untreated patients have a higher risk of cardiovascular diseases such as heart failure or stroke. According to studies, the prevalence rate of OSA among middle-aged men and women is 5% and 2-3% respectively.
Dr Jason Chan Ying-kuen, Associate Professor in the Department of Otorhinolaryngology, Head and Neck Surgery at CU Medicine, said, “Continuous positive airway pressure therapy is often used to treat OSA patients. They wear a device that introduces positive airway pressure into their airways to stent them open, but poor adherence has been reported worldwide due to device-related issues, such as air leaks, and patients’ clinical conditions, such as nasal congestion.”
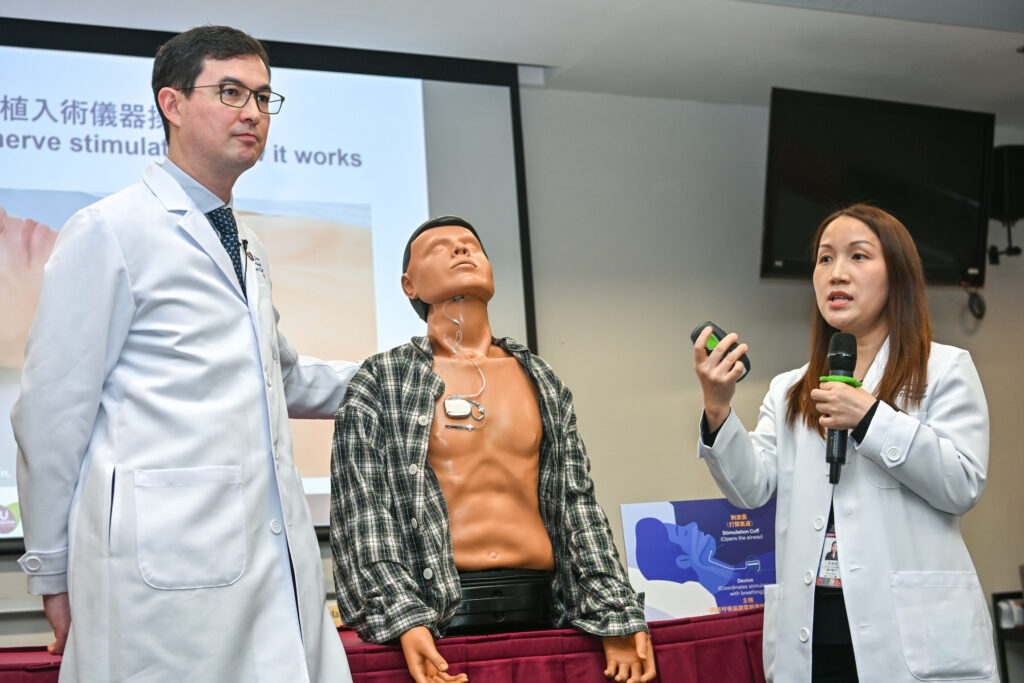
UAS therapy has become an emerging option for patients with moderate-to-severe OSA who fail to adhere to continuous positive airway pressure therapy. A neurostimulator the size of a pacemaker is implanted below the clavicle. It delivers stimulating electrical pulses to the hypoglossal nerve so as to activate the genioglossus muscle of the tongue and dilate patients’ pharynx while they sleep. The procedure is synchronised with ventilation, in particular inspiration detected by a sensing lead placed at the fourth intercostal region.
UAS is a technically demanding surgical procedure which requires an experienced, multi-disciplinary team
Dr Natalie Leung Moon-wah, Clinical Associate Professor (honorary) in the Department of Otorhinolaryngology, Head and Neck Surgery at CU Medicine, said, “UAS therapy is well established in the United States, and has been proven to durably maintain the effect of improving airway stability during sleep, improving patients’ quality of life. As the device is implanted in the body, patients have nothing they need to wear during sleep. However, it is a technically demanding surgical procedure, as the hypoglossal nerve is among the most delicate in the human body, responsible for motor innervation of the vast majority of the muscles in the tongue. The surgery requires a fully committed, experienced, multi-disciplinary team including sleep technician, anaesthetist, intensive care team and theatre nurses for the complicated post-operative and follow-up procedures.”
CU Medicine’s Otorhinolaryngology, Head and Neck Surgery team has completed three cases as of today, with satisfactory results. The apnoea-hypopnea index, a count of the number of upper airway obstructions per hour of sleep, measures the severity of OSA. Results showed an average 77% drop in the apnoea-hypopnea index among patients who received UAS therapy, with their combined average number of apnoeas and hypopneas per hour of sleep dropping from 44 to 10.3, meaning their OSA conditions improved from severe to mild.
Dr Jason Chan added, “Support from the Alice Ho Miu Ling Nethersole Charity Foundation has subsidised patients to receive this novel treatment. Many OSA patients have been long bothered by the condition and have lacked an effective remedy. We wish to help with training UAS teams so that it can become a more accessible procedure for OSA patients.”

CU Medicine introduced upper airway stimulation (UAS), an emerging surgical procedure, for obstructive sleep apnoea (OSA) patients who have problems accepting or adhering to standard continuous positive airway pressure treatment. With the support from the Alice Ho Miu Ling Nethersole Charity Foundation subsidising patients to receive this novel treatment, the team has completed three cases and successfully improved the patients’ condition. (From left) Dr Eddy Wong Wai-yeung, Clinical Associate Professor (honorary) in the Department of Otorhinolaryngology, Head and Neck Surgery at CU Medicine and Chief of Service of the Department of Ear, Nose and Throat at Prince of Wales Hospital; Mr Wilson Y.S. Mok, Chairman of the Board of Governors at Alice Ho Miu Ling Nethersole Charity Foundation; Dr Jason Chan Ying-kuen and Dr Natalie Leung Moon-wah, Associate Professor and Clinical Associate Professor (honorary) in the Department of Otorhinolaryngology, Head and Neck Surgery at CU Medicine; and Mr Leung, OSA patient who has received UAS.

Dr Jason Chan says poor adherence to continuous positive airway pressure therapy often happened to OSA patients. It may be due to device-related issues, such as air leakage, and patients’ clinical conditions, such as nasal congestion. These patients may have to seek surgical treatment.
Dr Natalie Leung explains, patients can use the remote control to adjust the voltage of electric stimulation from the UAS device to have an effective and comfortable treatment.

Mr Leung had been suffering from OSA for years without an effective treatment until he received UAS therapy last year. He says it took a short time for him to adapt to the automatic movement of the tongue after surgery. He soon got used to the system and was pleased with the treatment result.