CUHK
News Centre
CU Medicine finds surgical treatment lowers blood pressure in
children with severe obstructive sleep apnoea
But postoperative weight control is equally important
Childhood obstructive sleep apnoea (OSA) is a prevalent clinical condition and a risk factor for elevated blood pressure and hypertension in young adults. Surgical intervention is the recommended first-line treatment for OSA but its effect on blood pressure has been unclear. The Chinese University of Hong Kong’s (CUHK) Faculty of Medicine (CU Medicine) conducted the world’s first randomised controlled trial to evaluate the effect of surgical intervention on ambulatory blood pressure[i] in non-obese children with OSA. Results show that surgical treatment led to significant improvements in ambulatory blood pressure in children with more severe OSA, but not in those with less severe disease. However, the improvement in blood pressure was partially masked by weight gain following surgery.
Experts at CU Medicine remind the public that surgical intervention alone is insufficient for the effective management of OSA and its consequences: lifestyle changes and weight control are equally important. Study details have been published in the medical journal Sleep Medicine.
One-fifth of tested children in hospital found to have severe OSA
A previous CU Medicine study estimated that 5% of primary school-aged children in Hong Kong are affected by OSA. Snoring, night sweats and mouth breathing are among the common symptoms of OSA. There is one severe OSA case in every five children who undergo sleep tests at the Prince of Wales Hospital every year.
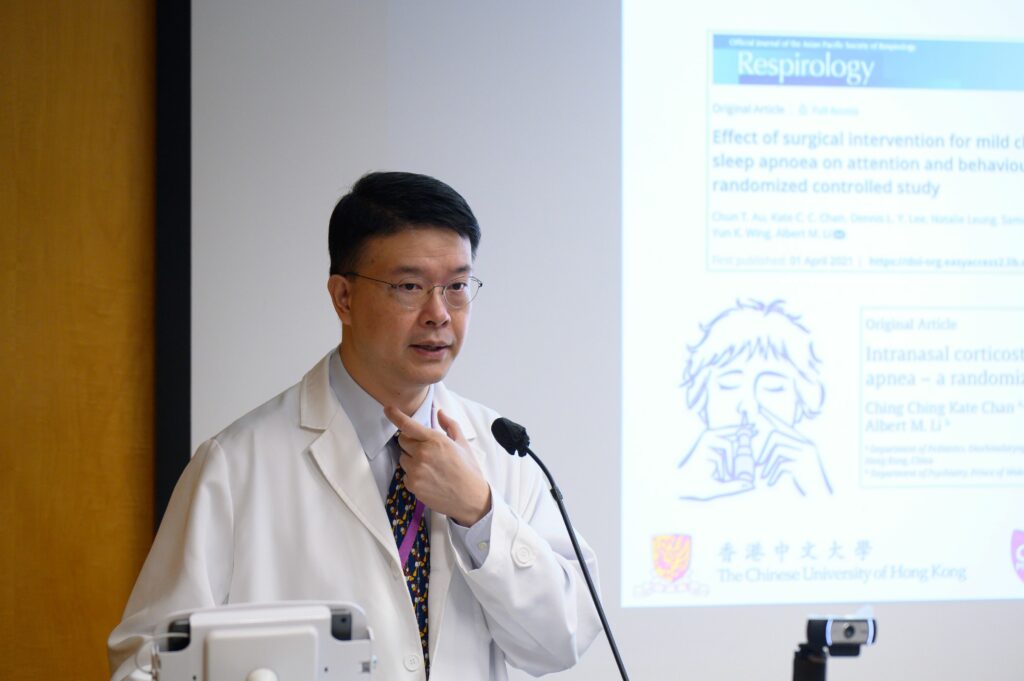
Professor Albert Martin Li, Chairman of the Department of Paediatrics at CU Medicine, stated, “This is noteworthy because OSA is a known risk factor for neurocognitive deficits, including poor attention and misbehaviour. It is also related to cardiovascular abnormalities like elevated blood pressure and even hypertension, which can lead to the future development of atherosclerosis.”
Enlarged tonsils and adenoids are a common cause of childhood OSA. Surgical intervention is the recommended first-line treatment for the condition. Dr Jun Au Chun-ting, Adjunct Assistant Professor in CU Medicine’s Department of Paediatrics, added, “Children with severe OSA benefit from early surgical intervention in terms of symptoms and behaviour. It is also important to confirm if the blood pressure of children with OSA improves following surgical intervention.”
Surgical intervention effectively manages blood pressure in severe OSA cases but not in less severe ones
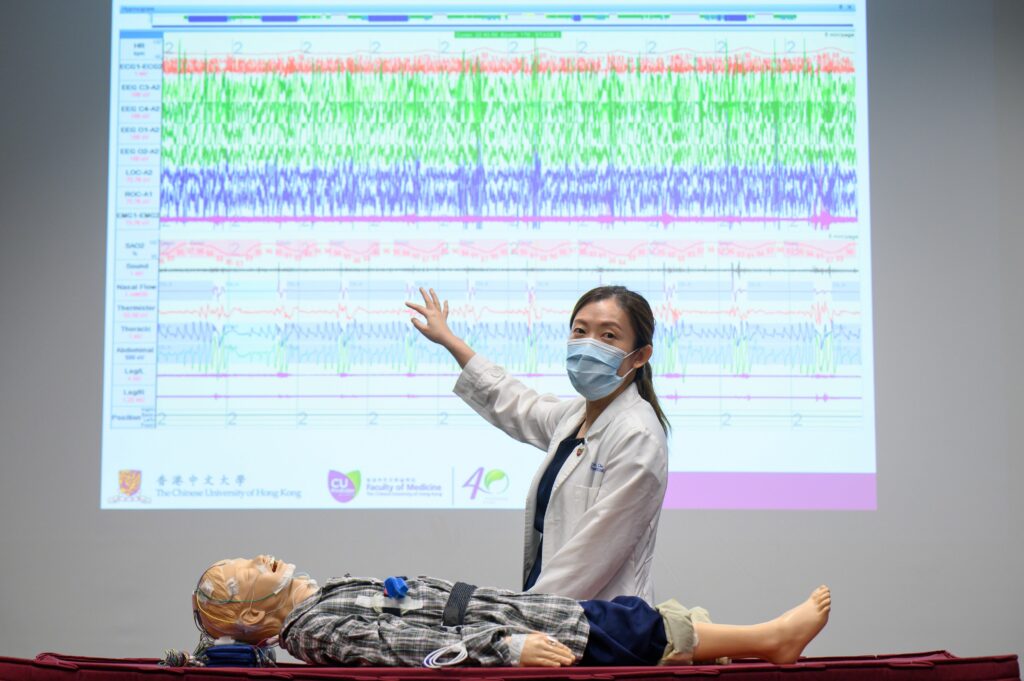
CU Medicine’s recent randomised clinical trial recruited 109 non-obese children aged 6 to 11 years who attended the chest and sleep disorder clinic with symptoms suggestive of OSA. All of them underwent a sleep test and were examined by otorhinolaryngologists. Changes in their daytime, nighttime and 24-hour average ambulatory blood pressure were recorded at baseline and nine months after a randomly assigned intervention of either early surgery or watchful waiting. Subjects were divided into mild-to-moderate and severe groups.
Results show that surgical treatment of OSA with reference to watchful waiting significantly reduced OSA severity. After surgery, the average number of obstructive respiratory events per hour during sleep decreased by 19, from an average of 23, in severe OSA cases, showing that most cases changed from severe to mild-to-moderate condition. An improvement in nighttime diastolic blood pressure was also observed in children with severe OSA. They experienced the largest decrease in their Z score, which measures the deviation between the blood pressure of subjects and the average blood pressure of people of the same gender and height. However, this effect was not observed in those with less severe disease.
On the other hand, the early surgery group had a greater increase in Body Mass Index (BMI) than the other group. This increase in BMI paralleled the increase in daytime systolic blood pressure, meaning that the improvement in blood pressure from early surgery was partially masked by weight gain. Details can be found in tables 1 and 2 in the appendix.
Lifestyle changes and weight control are equally important in managing OSA
Dr Kate Chan Ching-ching, Associate Professor at CU Medicine’s Department of Paediatrics, concluded, “The unfavourable weight gain in children with OSA following surgery may be explained by the alleviation of the breathing difficulty during sleep and hence reducing the related energy expenditure. As the increase in BMI can mask the beneficial effect on blood pressure outcomes, parents of children with OSA should be aware that there is a potential risk of weight gain after treatment. Clinicians should also provide advice about weight management, such as healthy diet and regular physical activity, after surgical treatment for OSA.”
[i] Note: Capturing nighttime blood pressure and the percentage drop of blood pressure from daytime to nighttime by 24-hour ambulatory monitoring is believed to be more sensitive and specific. It helps evaluate the adverse effects of OSA on the cardiovascular system.

CU Medicine conducted the world’s first randomised controlled trial to evaluate the effect of surgical intervention on ambulatory blood pressure in non-obese children with OSA. Results show that surgical treatment led to significant improvements in ambulatory blood pressure in children with more severe OSA, but not in those with less severe disease. However, the improvement in blood pressure was partially masked by weight gain following surgery.
The research team includes Dr Kate Chan, Associate Professor (left); Dr Jun Au, Adjunct Assistant Professor (zoom image on screen); and Professor Albert Li, Chairman, of the Department of Paediatrics at CU Medicine.