CUHK
News Centre
CU Medicine identifies a “fish allergenicity ladder” system
Promoting evidence-based, personalised seafood avoidance for fish allergy patients
Fish allergy is a common food allergy, with patients tending to avoid all kinds of fish. A study conducted by The Chinese University of Hong Kong (CUHK)’s Faculty of Medicine (CU Medicine) found that 40% of fish-allergic individuals reported tolerance of at least one type of fish, related to the level of β-parvalbumin, a kind of protein in the fish’s flesh. As a result, the research team was able to identify a “fish allergenicity ladder” system based on the clinical tolerance pattern, corresponding to β-parvalbumin levels in different fish. This system promotes precision medicine by allowing allergists to customise fish recommendations for patients. The team also found that many fish-allergic subjects were able to tolerate other seafood such as shrimps, crabs and clams. These findings promote personalised seafood avoidance based on the evidence from allergy tests. Study details have been published in The Journal of Allergy and Clinical Immunology: In Practice.
An unmet need to develop more precise diagnostic strategies and personalised recommendations tailored for fish-allergic patients
Fish allergy has an early onset during the first two to three years of life, and tends to persist at least until the teenage years. Allergic reactions range from mild skin or gastrointestinal symptoms to life-threatening breathing difficulties and anaphylaxis. Despite some fish-allergic patients reporting a history of tolerance of some fish, they are often labelled with the umbrella term fish-allergic and advised to avoid all types of fish.
Professor Leung Ting-fan, Alice Ho Miu Ling Nethersole Charity Foundation Professor of Paediatrics at CU Medicine, stated, “Fish is a highly nutritious food; it contains crucial nutrients such as protein and omega-3s that are essential for the growth of children. There is an unmet need to effectively assess patients for selective tolerance to fish in daily practice, so that they can be offered appropriate and safe clinical advice.”
The allergy team at CU Medicine, led by Professor Leung, recruited 249 fish-allergic children with a median age of 4.2 years. All participants underwent skin prick tests and measurement of specific IgE levels, an allergy-associated antibody, in response to a number of fish, while their clinical history and seafood consumption patterns after their initial allergic reactions to fish were recorded.
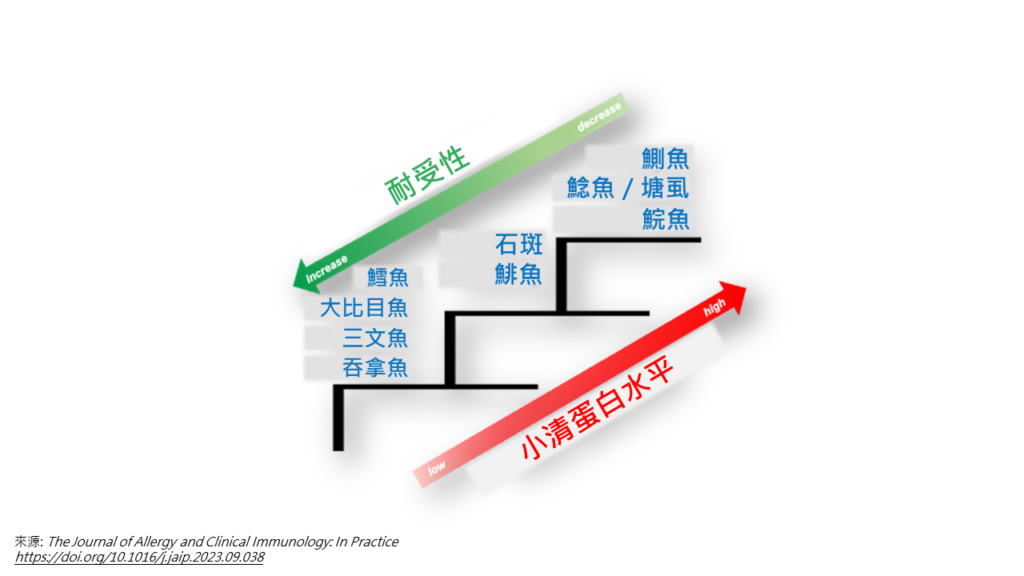
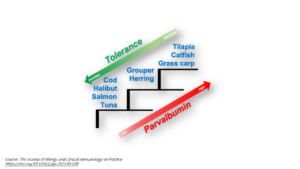
Study findings showed that 40% of fish-allergic participants indicated tolerance to certain fish species. Through the analysis of different fish-specific IgE levels, the team found the participants’ clinical tolerance pattern and identified a “fish allergenicity ladder” system. They found that tilapia, catfish and grass carp had the highest degree of allergenicity, followed by grouper and herring with an intermediate degree of allergenicity, and then by cod, halibut, salmon and tuna with the lowest degree of allergenicity.
Dr Christine Wai Yee-yan, Research Assistant Professor in the Department of Paediatrics at CU Medicine, explained, “The allergenicity of different fish species varies corresponding to the β-parvalbumin levels present in their flesh. The allergenicity ladder system identified by our team provides allergists with a significant reference to minimise the risk of adverse reactions during oral food challenges for fish allergy diagnosis, by choosing fish with lower level of β-parvalbumin to start the test. These fish-allergic children may then have fish species with low β-parvalbumin content reintroduced to their diets.”
Dr Agnes Leung Sze-yin, Assistant Professor in the Department of Paediatrics at CU Medicine, added, “Fish-allergic reactions like airway obstruction from anaphylactic shock can be life-threatening. It is recommended that individuals with selective fish tolerance consume fish they can tolerate in incremental amounts after thorough allergy evaluation, under careful supervision by allergists. It is also better for them to consume fish they can tolerate at home, where they can prepare and cook the fish carefully to avoid contamination with fish that have higher allergenicity.”
Shellfish avoidance is common in non-shellfish-sensitised individuals
While almost half of the fish-allergic individuals avoided all types of shellfish, such as shrimp, crab, clam and scallop, due to the mistaken belief that they are allergic to both, 33% of them lacked shellfish sensitisation. Professor Leung concluded, “Our study provides evidence that a considerable proportion of fish-allergic individuals exhibit selective tolerance to fish types with lower allergenicity. Many patients with fish allergies may also tolerate shellfish. They can be advised to consume different shellfish types, which will significantly improve their nutritional intake and quality of life. These findings underscore the importance of developing precise diagnostic strategies and providing clinical advice based on evidence from tests for seafood allergies to reduce unnecessary shellfish and fish avoidance.”

The allergy team at CU Medicine has identified a “fish allergenicity ladder” system based on the clinical tolerance pattern of fish allergy patients, corresponding to β-parvalbumin levels in different fish. This system promotes precision medicine by allowing experts in treating allergy to customise fish recommendations for patients.
(From left) Dr Christine Wai, Research Assistant Professor; Professor Leung Ting-fan, Alice Ho Miu Ling Nethersole Charity Foundation Professor of Paediatrics; and Dr Agnes Leung, Assistant Professor, from the Department of Paediatrics at CU Medicine.

Professor Leung Ting-fan advises that individuals with selective fish tolerance consume fish they can tolerate in incremental amounts after thorough allergy evaluation and under careful supervision in clinics. This is because fish-allergic reactions like anaphylactic shock can be life-threatening, which patients need immediate injection of medication like the adrenaline shown on his hand.

Dr Agnes Leung states that the current study found 40% of fish-allergic individuals reported tolerance of at least one type of fish, such as salmon and tuna which are of lower allergenicity level, and many fish-allergic subjects can tolerate shellfish. These findings underscore the importance of developing precise diagnostic strategies and providing clinical advice based on evidence from tests for seafood allergies to reduce unnecessary shellfish and fish avoidance.

Dr Christine Wai explains that the allergenicity of different fish species varies corresponding to the β-parvalbumin levels present in their flesh. β-parvalbumin-rich fish such as grass carp and catfish have the highest degree of allergenicity.