CUHK
News Centre
CU Medicine and PWH pioneer low-field MRI technology to launch Hong Kong’s first one-stop acute stroke management model
The Chinese University of Hong Kong (CUHK)’s Faculty of Medicine (CU Medicine) and the Prince of Wales Hospital (PWH), in collaboration with the Chinese Stroke Association and the Beijing Tiantan Hospital, affiliated to Capital Medical University, have introduced the use of 0.23T low-field magnetic resonance imaging (MRI) technology in Hong Kong as part of a nationwide, multicentre clinical trial of a new one-stop acute stroke management model, the Emergency Stroke Unit (ESU). Since its launch in August this year, the team has performed low-field MRI examinations on over twenty patients at PWH with promising results. The research team believes that this innovative technology has the potential to significantly improve the diagnostic and treatment processes for acute stroke patients. The clinical study is divided into two phases, with a target of enrolling 200 patients.
ESU model significantly reduces the time to treatment and improves patient outcomes
Stroke is the second-leading global cause of death and the most common cause of adult long-term physical disability. In Hong Kong, over 10,000 acute stroke cases are admitted to public hospitals annually, with nearly 80% being ischemic strokes, which occur when the blood flow to the brain is blocked. Without treatment, brain cells die at an alarming rate of 1.9 million every minute from stroke onset. Therefore, timely treatment is critical to dissolve or remove the blood clots and restore the blood flow to the brain through intravenous thrombolysis or endovascular thrombectomy.
Currently, for patients presenting at an Accident and Emergency Department with suspected stroke, the stroke team performs urgent treatment eligibility assessments, including reviewing medical history, arranging computed tomography (CT) scans, determining the type and location of the stroke, preparing blood tests and electrocardiograms, and conducting visual and motor assessments. Patients are then sent to a different location to receive treatment after diagnosis. To further reduce the time taken by diagnosis and treatment, the Chinese Stroke Association initiated a nationwide, multicentre clinical study in 2024, to evaluate the ESU model integrating low-field MRI technology. By consolidating clinical evaluation, imaging and treatment in a single treatment room equipped with a low-field MRI system, stroke patients can receive more streamlined and expedited care, potentially improving outcomes.
CUHK and PWH are participating in this 18-month clinical study as Hong Kong’s first pilot site. The ESU model utilises the innovative 0.23T low-field MRI technology, allowing neurologists to rapidly identify ischemic and hemorrhagic strokes within nine minutes and to detect large vessel occlusions so that patients can receive immediate clinical evaluation and treatment after the imaging examination.
Professor Meng Xia, Director of the Project Management Department at China National Clinical Research Center for Neurological Diseases, remarked: “Based on the experience of other stroke centres in mainland China participating in the study, the introduction of the ESU model has reduced the door-to-needle time to an average of 20 minutes, significantly faster than the 60-minute international guideline, bringing immense benefits to patients. We look forward to strengthening exchanges with Hong Kong in areas like nurturing talent, clinical research and cross-border research collaboration, in order to jointly promote scientific research and development.”
Professor Philip Chiu Wai-yan, Dean of CU Medicine, added: “This research not only helps improve acute stroke management but also strengthens the collaboration between medical institutions in Hong Kong and mainland China, promoting exchanges in research, education, innovation and technology transfer, and making significant contribution to patient well-being.”
Dr Chung Kin-lai, Cluster Chief Executive of New Territories East and Hospital Chief Executive of PWH, stated: “This collaborative research marks an important milestone towards accomplishing our mission of advancing innovative medicine and improving patient outcomes. Integrating this innovative technology into the acute stroke management workflow will potentially transform triage and treatment strategies.”
Low-field MRI allows greater flexibility and mitigates technical limitations of traditional imaging
The 0.23T low-field MRI system offers several advantages over the standard 1.5T or 3.0T MRI systems, including greatly enhanced flexibility, lower cost, smaller footprint, improved safety, no special shielding requirements, fewer metal object restrictions and standard power supply connectivity.
The research team at the Beijing Tiantan Hospital, affiliated to Capital Medical University found the low-field MRI demonstrated over 96% accuracy and 97% sensitivity in detecting ischemic lesions, compared to the 3.0T MRI. Additionally, compared with CT scans, the low-field MRI technology has higher certainty in visualising small or early ischemic changes. This breakthrough low-field MRI technology not only offers greater flexibility compared with traditional systems but also holds immense potential to significantly improve the diagnostic and treatment pathways for stroke patients.
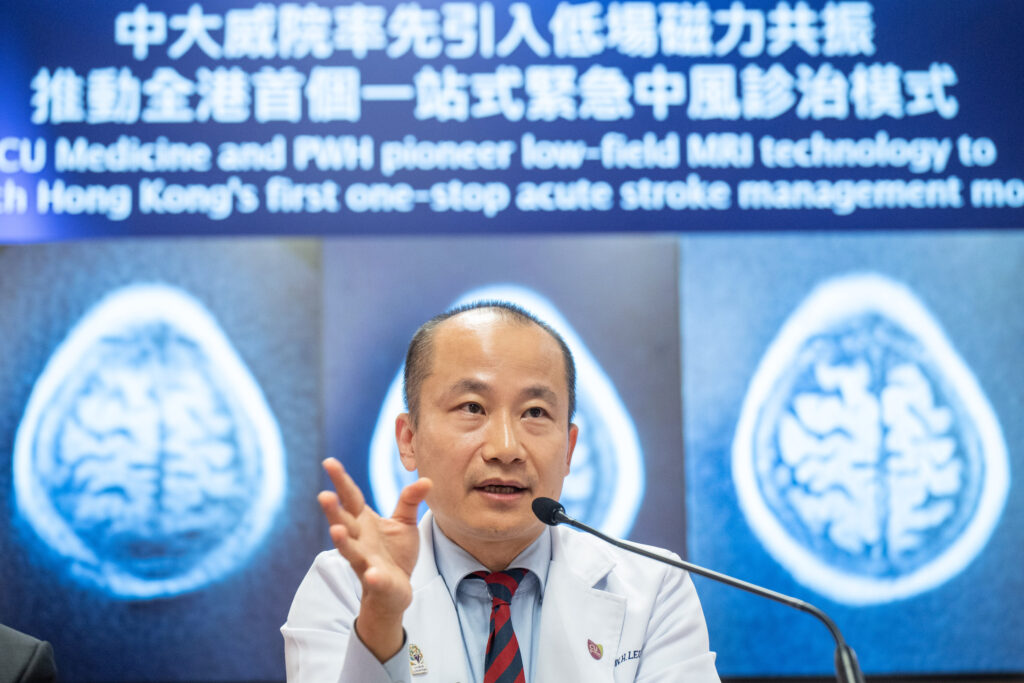
Professor Thomas Leung Wai-hong, Lee Quo Wei Professor of Neurology and Head of the Division of Neurology in CU Medicine’s Department of Medicine and Therapeutics; and Director and Honorary Consultant of the Acute Stroke Unit at PWH, hopes the result of the clinical study will not only advance stroke research but also facilitate the clinical application of the ESU model in Hong Kong. Professor Leung concluded: “With the rapidly ageing population, we anticipate an increasing incidence of acute stroke cases. Timely treatment is crucial for reducing mortality and morbidity. The ESU model can significantly expedite the door-to-needle and door-to-groin puncture time, marking a new milestone in acute stroke treatment that could be a game-changer, benefiting more patients.”

The Chinese University of Hong Kong (CUHK)’s Faculty of Medicine (CU Medicine) and the Prince of Wales Hospital (PWH), in collaboration with the Chinese Stroke Association and the Beijing Tiantan Hospital, affiliated to Capital Medical University, have introduced the use of 0.23T low-field magnetic resonance imaging (MRI) technology to launch Hong Kong’s first one-stop acute stroke management model.
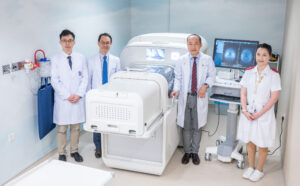
(From left) Dr Ma Sze-ho, Clinical Associate Professor (Honorary), Division of Neurology in CU Medicine’s Department of Medicine and Therapeutics, and Associate Consultant at PWH’s Department of Medicine and Therapeutics; Professor Thomas Leung Wai-hong, Lee Quo Wei Professor of Neurology and Head of the Division of Neurology in CU Medicine’s Department of Medicine and Therapeutics, and Director and Honorary Consultant of the Acute Stroke Unit at PWH; Professor Philip Chiu Wai-yan, Dean of CU Medicine; Professor Meng Xia, Director of the Project Management Department at China National Clinical Research Center for Neurological Diseases; Professor Jing Jing, Associate Director, Tiantan Neuroimaging Center of Excellence, China National Clinical Research Center for Neurological Diseases, Beijing Tiantan Hospital, affiliated to Capital Medical University; Dr Chung Kin-lai, Cluster Chief Executive of New Territories East and Hospital Chief Executive of PWH; Dr Raymond Cheng Chi-hung, Chief of Service (Accident and Emergency), PWH; Dr Cindy Leng, Assistant Professor, Department of Medicine and Therapeutics, CU Medicine

The Chinese Stroke Association initiated a nationwide, multicentre clinical study in 2024, to evaluate the Emergency Stroke Unit (ESU) model integrating low-field MRI technology. CUHK and PWH are participating in this 18-month clinical study as Hong Kong’s first pilot site. The clinical study is divided into two phases, with a target of enrolling 200 patients.
(From left) Dr Ma Sze-ho, Clinical Associate Professor (Honorary), Division of Neurology in CU Medicine’s Department of Medicine and Therapeutics, and Associate Consultant at PWH’s Department of Medicine and Therapeutics; Professor Thomas Leung Wai-hong, Lee Quo Wei Professor of Neurology and Head of the Division of Neurology in CU Medicine’s Department of Medicine and Therapeutics, and Director and Honorary Consultant of the Acute Stroke Unit at PWH; Professor Philip Chiu Wai-yan, Dean of CU Medicine; Professor Meng Xia, Director of the Project Management Department at China National Clinical Research Center for Neurological Diseases; Professor Jing Jing, Associate Director, Tiantan Neuroimaging Center of Excellence, China National Clinical Research Center for Neurological Diseases, Beijing Tiantan Hospital, affiliated to Capital Medical University; Dr Chung Kin-lai, Cluster Chief Executive of New Territories East and Hospital Chief Executive of PWH; Dr Raymond Cheng Chi-hung, Chief of Service (Accident and Emergency), PWH; Dr Cindy Leng, Assistant Professor, Department of Medicine and Therapeutics, CU Medicine
Professor Thomas Leung Wai-hong highlights: “Timely treatment for acute stroke is crucial for reducing mortality and morbidity. The ESU model can significantly expedite the door-to-needle and door-to-groin puncture time, marking a new milestone in acute stroke treatment that could be a game-changer, benefiting more patients.”

Ms Chiu, a stroke patient, was able to receive timely treatment after a low-field MRI examination which revealed the location of her ischemic stroke and her suitability for thrombolytic therapy, significantly enhanced the clinical outcomes.
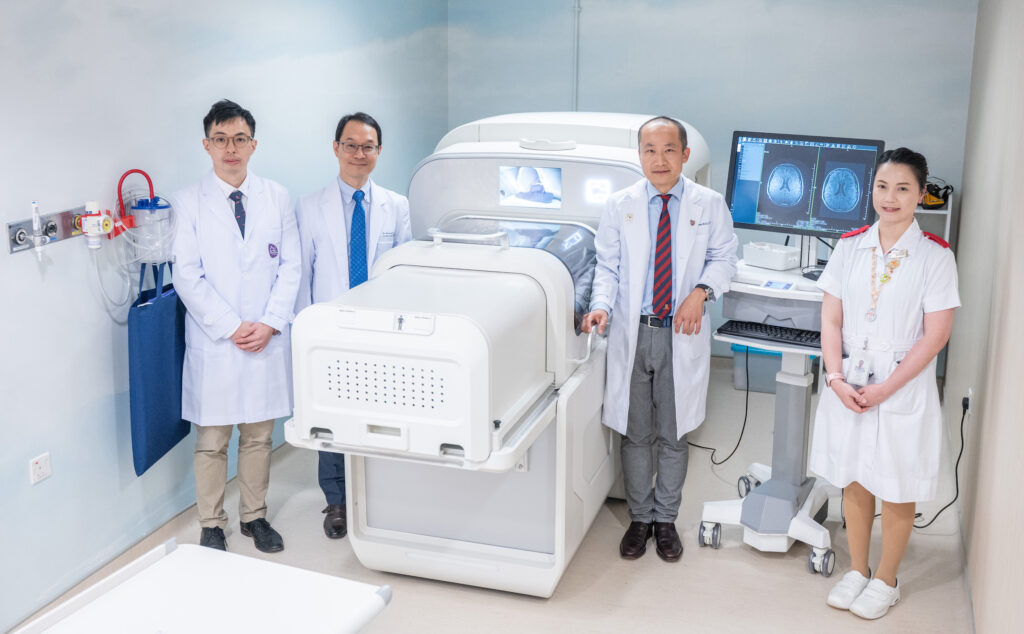
Under the ESU model, clinical evaluation, imaging and treatment can be conducted in a single treatment room equipped with a low-field MRI system. Stroke patients can receive more streamlined and expedited care, potentially improving outcomes.
(From left) Dr Ma Sze-ho, Clinical Associate Professor (Honorary), Division of Neurology in CU Medicine’s Department of Medicine and Therapeutics, and Associate Consultant at PWH’s Department of Medicine and Therapeutics; Dr Raymond Cheng Chi-hung, Chief of Service (Accident and Emergency), PWH; Professor Thomas Leung Wai-hong, Lee Quo Wei Professor of Neurology and Head of the Division of Neurology in CU Medicine’s Department of Medicine and Therapeutics, and Director and Honorary Consultant of the Acute Stroke Unit at PWH; Ms Maggie Lau, Nurse Consultant (Stroke), PWH

The low-field MRI demonstrated over 96% accuracy and 97% sensitivity in detecting ischemic lesions. Additionally, compared with CT scans, the low-field MRI technology has higher certainty in visualising small or early ischemic changes. This breakthrough low-field MRI technology holds immense potential to significantly improve the diagnostic and treatment pathways for stroke patients.

The 0.23T low-field MRI system offers several advantages over the standard MRI systems, including greatly enhanced flexibility, lower cost, smaller footprint, improved safety, no special shielding requirements, fewer metal object restrictions and standard power supply connectivity.