CUHK
News Centre
CUHK and Queen Mary University of London lead largest international trial of time-lapse imaging systems for embryo incubation in IVF
Technology found to enjoy no advantage over conventional methods
An international trial of time-lapse imaging (TLI) systems for embryo incubation and selection during in vitro fertilisation (IVF), co-led by the Assisted Reproductive Medicine Unit in the Department of Obstetrics and Gynaecology at The Chinese University of Hong Kong (CUHK)’s Faculty of Medicine (CU Medicine) and the Women’s Health Research Unit at Queen Mary University of London, has found that a TLI system gives no advantage in clinical outcomes over conventional methods although it offers a seamless process for monitoring embryo development. Researchers believe the findings provide insights that will allow for better allocation of resources and investment in future IVF services. The landmark findings of the largest international trial of its kind have been published in The Lancet.
Continuous debates over the clinical effectiveness of TLI systems
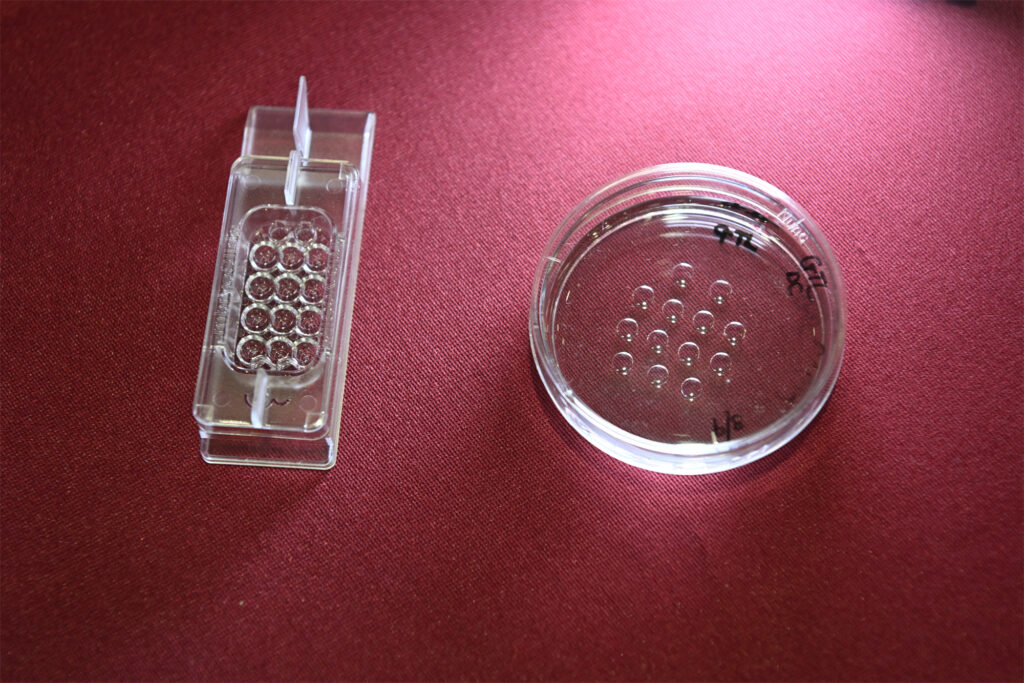
One out of six couples in Hong Kong experience fertility problems. IVF is the most common treatment allowing infertile couples to achieve pregnancy. Gametes from wife and husband are combined in an IVF laboratory to create the embryo, with a resulting good-quality embryo transferred to the mother’s womb, typically on the fifth day.
The conventional incubation method requires an embryologist to observe the embryo once per day. Moving the incubator in order to observe the embryo can potentially disturb the latter. In contrast, a TLI system, equipped with an internal camera for continuous observation without disturbance, offers a seamless monitoring process. While TLI has been a common practice in IVF labs for over a decade, its clinical effectiveness remains controversial. TLI systems are often associated with additional costs for patients due to high equipment expenses.
Professor David Chan Yiu-leung, an embryologist from the Department Obstetrics and Gynaecology at CU Medicine, and Dr Priya Bhide, an expert in reproductive medicine from Queen Mary, led this three-arm, parallel-group, double-blind, randomised, controlled trial of 1,500 participants undergoing IVF at seven centres in Hong Kong and the UK. Hong Kong contributed to one-third of the cases in this study. One group of participants received TLI-based embryo selection, one received standard static assessment using undisturbed culture and a third received conventional assessment using a light microscope and standard embryo culture in standard incubators. Results showed no significant difference among three groups in the live birth rates for embryos and clinical pregnancy rates. (Please refer to Appendix for details.)
Professor Liona Poon Chiu-yee, Chairperson of the Department of Obstetrics and Gynaecology at CU Medicine, said: “Our department encourages randomised controlled trial studies to support evidence-based medicine refuting hypothetical benefits without proven clinical outcomes. We are dedicated to providing accurate treatment choices and the highest level of care to our patients. The concept of ‘non-disturb culturing’ has been widely accepted as a better procedure by IVF specialists. This study proved that theoretical concepts of advanced technology do not always translate into improved clinical outcomes.”
Professor David Chan Yiu-leung, Assistant Professor in the Department of Obstetrics and Gynaecology at CU Medicine, said: “Although TLI is an important equipment in IVF labs, it does not improve IVF clinical outcomes. Patients seeking IVF treatment should be vigilant about fees for embryo culturing, as clinics might impose additional fees for the use of TLI.”
Dr Jacqueline Chung Pui-wah, Associate Professor in the Department of Obstetrics and Gynaecology at CU Medicine, said: “The findings from this study could prompt IVF clinics to reconsider how they allocate their budget for equipment. Instead of investing heavily in TLI machines, they could focus more on lab equipment that has a direct, measurable impact on live birth rates.”

An international trial of time-lapse imaging (TLI) systems for embryo incubation and selection during in vitro fertilisation (IVF), co-led by the Assisted Reproductive Medicine Unit in the Department of Obstetrics and Gynaecology at CU Medicine and the Women’s Health Research Unit at Queen Mary University of London, has found that a TLI system gives no advantage in clinical outcomes over conventional methods although it offers a seamless process for monitoring embryo development. The landmark findings of the largest international trial of its kind have been published in The Lancet. (From left) Professor Liona Poon Chiu-yee, Department Chairperson; Professor David Chan Yiu-leung, Assistant Professor; and Dr Jacqueline Chung Pui-wah, Associate Professor in the Department of Obstetrics and Gynaecology at CU Medicine.