CUHK
News Centre
International lung cancer study involving CU Medicine shows that a targeted therapy doubles the progression-free survival of advanced cancer patients, compared to standard treatment
The Chinese University of Hong Kong (CUHK)’s Faculty of Medicine (CU Medicine) joined the world’s first international study to investigate the effect of a targeted therapy on newly diagnosed advanced or metastatic non-small-cell lung cancer (NSCLC) patients. For NSCLC patients who are rearranged during transfection (RET) fusion-positive, a driver of lung cancer, the medicine demonstrated a significantly improved mean progression-free survival rate, more than double that of people who received the current first-line standard treatment.
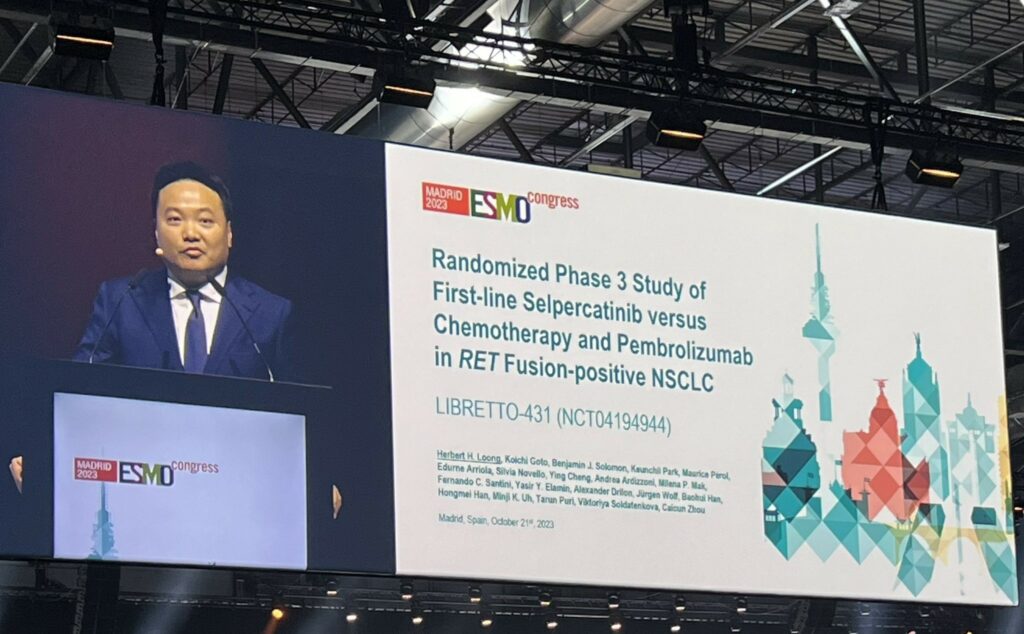
The study results showed that targeted therapy can be the first-line standard of care in untreated RET fusion-positive advanced NSCLC patients. Dr Herbert Loong Ho-fung, a member of the international research team and Associate Professor from the Department of Clinical Oncology at CU Medicine, presented the results of this multinational clinical trial, involving China, Italy, Australia and South Korea etc., on behalf of fellow investigators at the European Society of Medical Oncology (ESMO) Congress on 21 October 2023. Details of the study have just been published in the leading international journal The New England Journal of Medicine.
The first randomised trial of a targeted agent versus immunotherapy plus chemotherapy in a biomarker-selected patient population
Lung cancer is the leading cause of cancer-related deaths worldwide. It is also the leading cause of cancer deaths in Hong Kong, with about 4,000 cases every year. NSCLC accounts for over 80% of all lung cancers. Epidermal Growth Factor Receptor (EGFR) gene mutation and Anaplastic Lymphoma Kinase (ALK) positive are common lung cancer drivers, while RET fusions have been identified in approximately 1% to 2% of all NSCLC cases.
For NSCLC patients who are EGFR or ALK negative, including those who are RET fusion-positive, platinum-based chemotherapy (cisplatin or carboplatin) plus pemetrexed with or without the immunotherapy drug pembrolizumab is the current first-line standard of care.
In this phase 3 study, a targeted therapy, selpercatinib, was used as an initial treatment for patients with RET fusion-positive advanced or metastatic NSCLC. Their treatment outcomes were compared to those of patients receiving the current first-line standard medicine. This study represents the first randomised trial of a targeted agent versus immunotherapy plus chemotherapy in a biomarker-selected patient population.
Study results highlight the importance of timely and comprehensive genomic testing for NSCLC patients
The study enrolled 212 patients with unresectable stage III to IV NSCLC at 103 study sites across 23 countries. They were randomly assigned to the targeted therapy group or the control group. Results showed that the median progression-free survival of the targeted therapy group was 24.8 months, more than double the 11.2 months of the control group. They also had a higher overall response rate, longer duration of response and significantly reduced central nervous system progression incidence rate. Adverse events observed from the targeted drug were generally consistent with those identified in previous reports. The details can be found in table 1 in the appendix.
Dr Loong stated, “Patients need the most effective therapies to be used early in treatment. Our study results support selpercatinib as the first-line standard of care for RET fusion-positive advanced NSCLC. The improved treatment outcomes also highlight the importance of timely and comprehensive genomic testing for RET fusions at the time of diagnosis to inform first-line therapy for this patient population.”

CU Medicine joined the world’s first international study to investigate the effect of a targeted therapy on newly diagnosed advanced or metastatic non-small-cell lung cancer (NSCLC) patients. For NSCLC patients who are rearranged during transfection (RET) fusion-positive, a driver of lung cancer, the medicine demonstrated a significantly improved mean progression-free survival rate, more than double that of people who received the current first-line standard treatment.

Featured in the photo is Dr Herbert Loong, Associate Professor from the Department of Clinical Oncology at CU Medicine, presenting the results of this multinational clinical trial on behalf of fellow investigators at the European Society of Medical Oncology (ESMO) Congress in Madrid, Spain. Details of the study have just been published in the leading international journal The New England Journal of Medicine.