CUHK
News Centre
CU Medicine proves a new ultrasound-guided endoscopic procedure has higher success and shorter procedural time for treating malignant distal biliary obstruction
- Placement of drainage stents through conventional endoscopic methods can be difficult if patient’s duodenum is fragile, distorted or narrowed.
- The new procedure allows direct creation of a connection between the bile duct and duodenum, similar to traditional surgery but without the associated risks and with improved outcomes.
Malignant distal biliary obstruction (MDBO) is a common condition in patients with unresectable pancreaticobiliary cancers or metastasis. The Chinese University of Hong Kong’s (CUHK) Faculty of Medicine (CU Medicine) was the first to introduce endoscopic ultrasound (EUS)-guided choledocho-duodenostomy (ECDS), a close-to-non-invasive technology, to treat MDBOs in patients in Hong Kong. A recent multicentre international study conducted by CU Medicine proved that this new ultrasound-guided endoscopic procedure is comparable to conventional endoscopic biliary drainage in unresectable MDBO. In addition, it has a significantly higher technical success rate and a shorter procedural time.
The study provides evidence to support the application of ECDS to patients as a first-line therapeutic modality, when placement of a stent in the bile duct through the tumour by conventional endoscopic methods may be difficult. The results have been published in the medical journal Gastroenterology.
MDBO is a common health condition in patients with unresectable pancreaticobiliary cancers
MDBO occurs when a malignant tumour invades the bile duct, causing obstruction; the symptoms include painless yellowish colouring of the skin and eyes (jaundice) and skin itchiness (pruritus). Percutaneous, endoscopic, and surgical biliary drainage are used for treating MDBOs in patients with unresectable disease. The conventional method of inserting a stent into the bile duct through endoscopic retrograde cholangiopancreatography (ERCP) and EUS-guided biliary drainage with metal stents are both available endoscopic options.
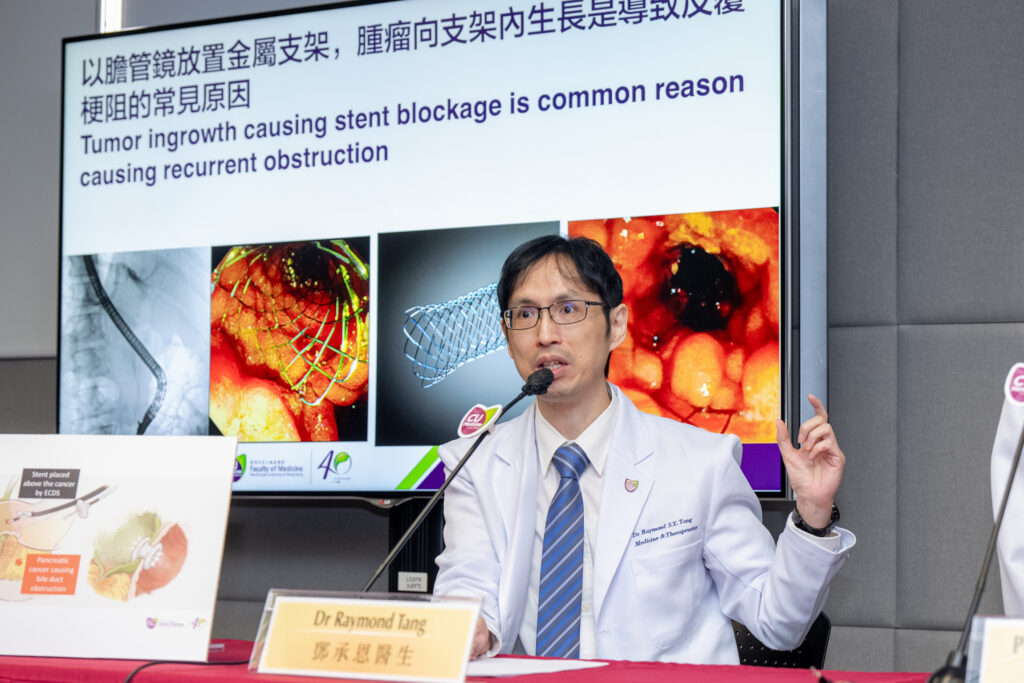
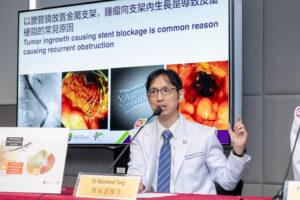
Dr Raymond Tang Shing-yan, Assistant Professor in the Department of Medicine and Therapeutics at CU Medicine, said, “Malignant distal biliary obstruction affects thousands of patients with advanced cancer in Hong Kong every year. In view of the current treatment options, EUS-guided biliary drainage, which allows insertion of a stent, similar to surgical bypass, has the advantages of reducing tumour ingrowth into the stent and potentially higher technical success with shorter procedural times.”
CU Medicine was the first to introduce the new procedure, known as ECDS, in Hong Kong
To further prove this, the CU Medicine research team conducted a randomised clinical trial with centres in France, Belgium, Denmark, Italy, Thailand and Australia. The study compared the outcomes of ERCP and ECDS, where the latter is one of the approaches to EUS-guided biliary drainage.
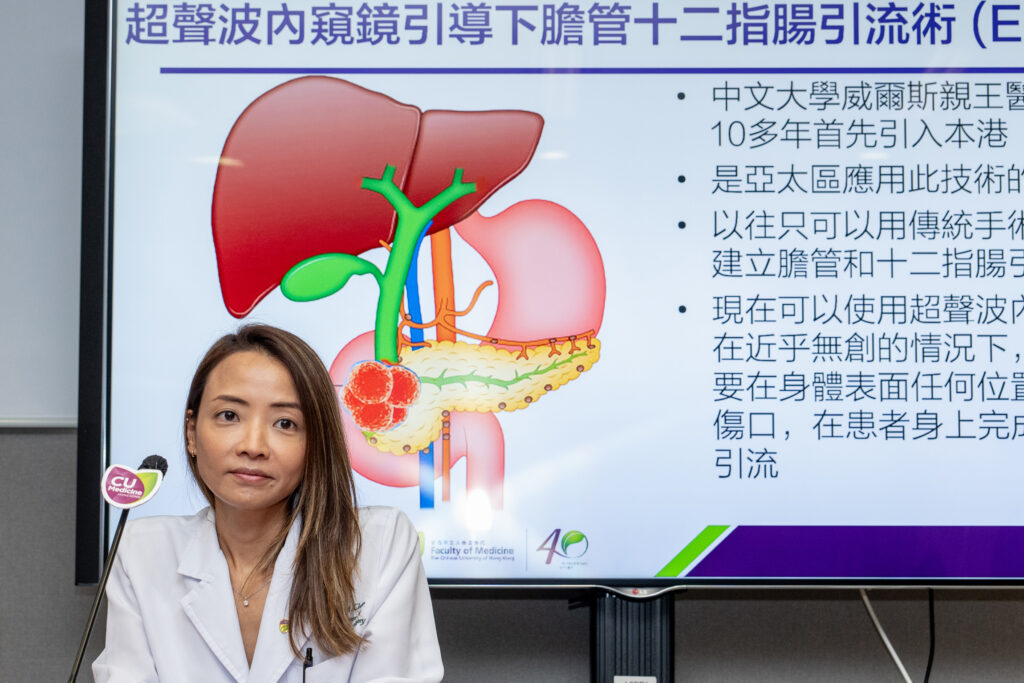
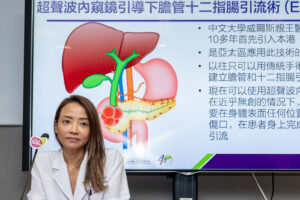
Dr Shannon Melissa Chan, Assistant Professor in the Department of Surgery at CU Medicine, stated, “We introduced ECDS in Hong Kong some 10 years ago and are one of the pioneers in the Asia-Pacific region. This close-to-non-invasive technology was first applied to patients at the Prince of Wales Hospital and is now increasingly adopted in public hospitals.”
The team recruited 155 patients for the study. Results showed that both ECDS and ERCP had a high one-year stent patency rate. Nevertheless, ECDS was associated with superior technical success and a shorter procedural time than ERCP. The details are summarised in the following table:
|
Outcomes |
ECDS group (79 patients) |
ERCP group (76 patients) |
|
*Technical success |
96.2% |
76.3% |
|
**Clinical success |
93.7% |
90.8% |
|
Procedural time |
10 mins |
25 mins |
|
30-day adverse events |
16.5% |
17.1% |
|
One-year stent patency rate |
91.1% |
88.1% |
*Technical success was defined as the placement of the metal stent across the stricture site.
**Clinical success was defined as the completion of stent placement with reduction of total serum bilirubin levels.
Professor Anthony Teoh Yuen-bun, Professor in CU Medicine’s Department of Surgery, explained, “There are several factors that make placement of stents endoscopically with ERCPs difficult. They include edema and friability in the duodenum due to malignancy, distortion and duodenum narrowing due to tumour infiltration. In these cases, ECDS is more advantageous because the procedure allows direct creation of a connection between the bile duct and duodenum, similar to traditional surgery while avoiding the need to create external wounds or drains. This close-to-non-invasive technology allows patients to avoid the risks of traditional surgery with improved outcomes. Furthermore, when compared to the conventional means of endoscopic drainage by ERCP, the procedure was associated with higher technical success and shorter procedural times improving the ease of stent placement.”
Professor Teoh said that both ECDS and ERCP could be options for primary biliary drainage in unresectable MDBO. As ECDS is associated with higher technical success and shorter procedural time, it is preferred when difficult ERCPs are anticipated.
The study details can be found at https://doi.org/10.1053/j.gastro.2023.04.016.
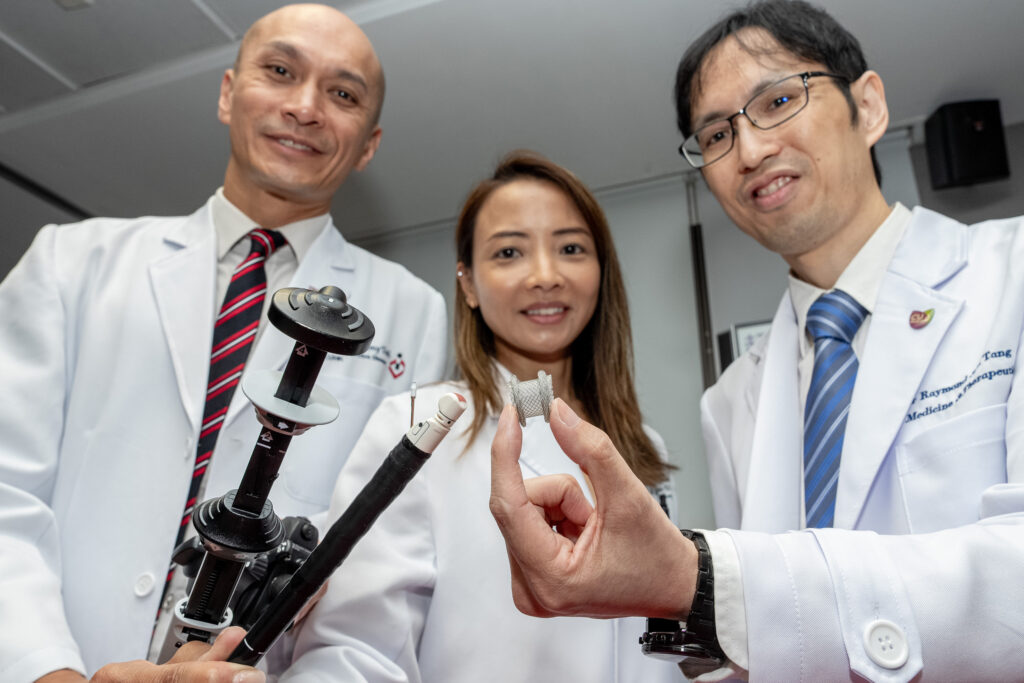
An international study conducted by CU Medicine proves that the outcome of endoscopic ultrasound (EUS)-guided Choledocho-duodenostomy (ECDS) is comparable to conventional endoscopic biliary drainage in unresectable malignant distal biliary obstruction (MDBO). Study results show that it has a significantly higher technical success rate and a shorter procedural time.
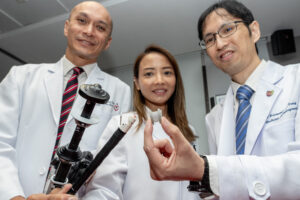
(From left) Professor Anthony Teoh, Professor; and Dr Shannon Chan, Assistant Professor, in the Department of Surgery; and Dr Raymond Tang, Assistant Professor in the Department of Medicine and Therapeutics, at CU Medicine.

Professor Anthony Teoh states that placement of drainage stents through conventional endoscopic methods can be difficult if patient’s duodenum is fragile, distorted or narrowed. ECDS is preferred in these cases.