CUHK
News Centre
CU Medicine uncovers the keys for liver cancer adaptation to immunotherapy
Pioneering new combination therapy in a Phase II clinical trial
Liver cancer remains one of the most common cancers in the world. Recent research from The Chinese University of Hong Kong (CUHK)’s Faculty of Medicine (CU Medicine) has discovered how liver cancer cells adapt to immunotherapy, the most advanced therapy for cancer patients. The team empowered immunotherapy by counteracting the resistance mechanisms of cancer cells and confirmed their clinical potential in liver cancer animal models. Research results have been published in the leading international journal Gut. The team is also going to commence a new Phase II clinical trial of combination immunotherapy, aiming to translate the discovery into patient benefits.
Recently, immunotherapy has increasingly been given to patients in the clinic. However, checkpoint inhibitors, the most used immunotherapy in liver cancer, can only benefit approximately 20% of patients. Moreover, patients who initially respond can become resistant during treatment.
New mouse models recapitulating human cold liver cancer enable identification of targets to improve immunotherapy
Immunotherapy-resistant liver cancer patients are associated with an immunosuppressive cold tumour microenvironment. However, the animal models commonly used in the laboratory do not reflect the complex organ-specific aspects of tumour development. Advances in modelling dynamic tumour-immune interactions are therefore critical to understand resistance mechanisms and improve immunotherapy.
Professor Alfred Cheng Sze-lok, Assistant Dean (Research) and Professor from the School of Biomedical Sciences (SBS) at CU Medicine, stated, “Our research team spent more than a year establishing two mouse models of immunotherapy resistance that recapitulate the immune landscape of human cold liver cancer. Coupling the new mouse models with the latest single-cell sequencing technology, we were able to discover new molecular pathways by which liver cancer cells circumvent the therapy-armed immune system. As we found these escape routes, we further developed roadblocks and successfully eliminated the cancer cells through combination immunotherapy.”
The new clinically relevant mouse models are instrumental in identifying and verifying actionable targets for therapeutic interventions. Dr Xiong Zhewen, Postdoctoral Fellow from the SBS at CU Medicine, said, “To construct these models, we continuously select immunotherapy-resistant cancer cells from the parental cells that are initially sensitive to the treatment. I am delighted to work out mouse models that can vividly mimic human liver cancer, leading to discoveries that break through existing scientific knowledge.”
The team applied bioinformatics to pinpoint PPARγ and class-I HDACs as the key regulatory proteins for promoting the cold tumour microenvironment. Professor Cheng added, “This is the first study to show that liver cancer cells adapt to immunotherapy through non-genetic mechanisms. Together with our colleagues in clinic, we are very pleased to determine the precision approaches that can overcome immunotherapy resistance.”
Bench-bedside research pioneers the development of next-generation immunotherapy
Professor Stephen Chan Lam, Assistant Dean (Health Systems) and Professor of the Department of Clinical Oncology at CU Medicine, commented, “Basic and clinician scientists must work hand-in-hand to accelerate breakthrough discoveries for effective cancer therapies. My close colleagues in the laboratory have the latest scientific technologies. As a doctor, I need to focus on how to translate the technologies to help patients. This work exemplifies the cohesiveness of CU Medicine in promoting health through innovation. Indeed, we found the same molecular alterations in liver cancer patients who are not responsive to checkpoint inhibitors, like the discoveries in the mouse models.”
Professor Zhou Jingying, Assistant Professor from the SBS at CU Medicine, added, “Immune cold tumours, characterised by T cell exclusion and dysfunction, represent a bottleneck for current immunotherapy. As we discover promising strategies that turn the cold tumour hot through this collaborative bench-bedside research, more patients can benefit from immunotherapy.”
The team has further used their new mouse models to demonstrate the effectiveness and safety of a novel class-I HDAC drug in combination with checkpoint inhibitors. Professor Stephen Chan remarked, “Based on the promising preclinical findings, we will initiate a Phase II clinical trial for liver cancer patients resistant to immunotherapy alone. We now have an opportunity to translate our research discovery into an effective and safe new generation of immunotherapy for patients with cold cancers.”
Enquiries regarding the new Phase II clinical trial (NCT05873244) can be made by phone at 3505-1042.

Recent research by CU Medicine has empowered immunotherapy by counteracting the resistance mechanisms of cancer cells and confirmed their clinical potential in liver cancer animal models. The team is also going to commence a new Phase II clinical trial of combination immunotherapy, aiming to translate the discovery into patient benefits.
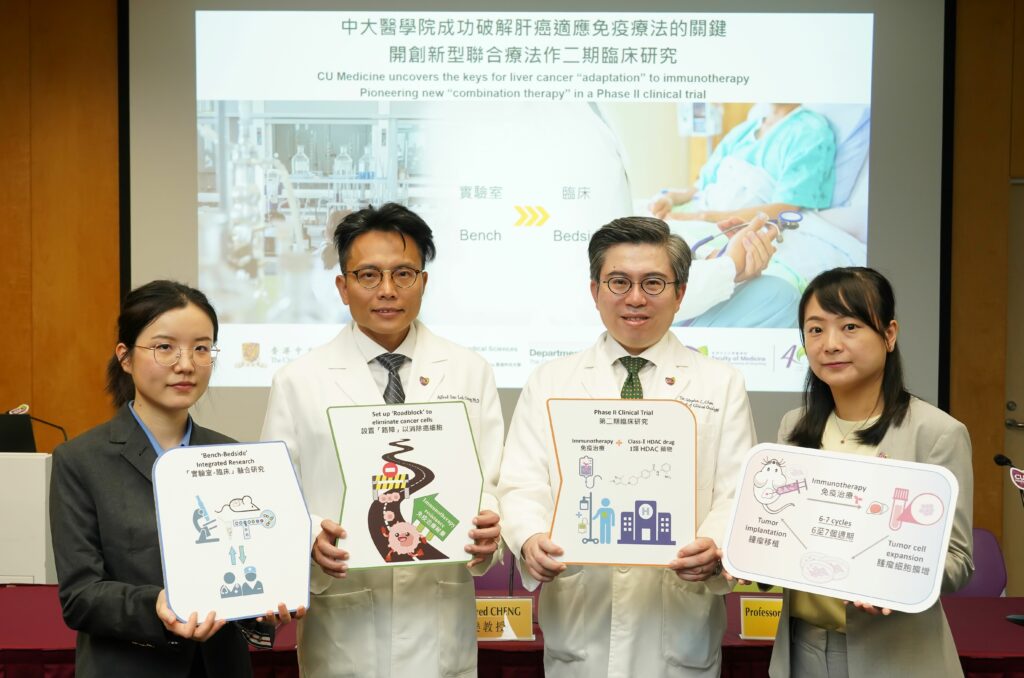
(From left) Dr Xiong Zhewen, Postdoctoral Fellow of the School of Biomedical Sciences (SBS); Professor Alfred Cheng, Professor of SBS; Professor Stephen Chan, Professor of the Department of Clinical Oncology; and Professor Zhou Jingying, Assistant Professor of SBS, at CU Medicine.

Professor Stephen Chan states that this “bench-to-bedside” research exemplifies the cohesiveness of CU Medicine in promoting health through innovation.

Professor Alfred Cheng explains that using the latest single-cell sequencing technology, the research team was able to discover new molecular pathways by which liver cancer cells circumvent the therapy-armed immune system. The team further developed roadblocks and successfully eliminated the cancer cells through combination immunotherapy.