CUHK
News Centre
CUHK discovers the occurrence of gut microbiome dysbiosis at the prodromal stages of Parkinson’s disease
Gives novel insights into neurodegenerative prevention, intervention and diagnosis
Parkinson’s disease (PD) is the second most common neurodegenerative disease worldwide. Early intervention reduces symptoms’ impact on patients. A study conducted by The Chinese University of Hong Kong’s (CUHK) Faculty of Medicine (CU Medicine) discovered that patients with rapid eye movement sleep behaviour disorder (RBD), a sleep disorder common in patients at the prodromal stages of PD, suffer gut microbiome dysbiosis similar to that of PD patients. In addition, the research team found that similar changes in gut microbes have already emerged in first-degree relatives of RBD patients. Notably, the abundance of health-promoting bacteria is depleted in their gut, while pro-inflammatory bacteria that could potentially disrupt intestinal barrier integrity are enriched.
Study results revealed that gut microbiome dysbiosis is a risk factor at the very early stage of PD, even occurring before the onset of RBD. This sheds light on the identification of high-risk prodromal PD cases by gut microbiome screening, as well as paving the way for early intervention, prevention and treatment of PD and other neurodegenerative diseases by targeting gut microbiome features. Study details have been published in the leading international journal Nature Communications.
Intestinal dysfunction may play a crucial role in early PD
In 2019, CU Medicine’s Department of Psychiatry conducted the world’s first in-person family RBD study. The study confirmed that first-degree relatives of RBD patients are three to six times of healthy controls to suffer from a series of neurodegenerative problems, including RBD, PD and dementia. Professor Liu Yaping, Adjunct Assistant Professor of the Department of Psychiatry at CU Medicine, said, “It is worth noting that relatives of RBD patients have a significantly higher incidence of constipation, suggesting that intestinal dysfunction may play a key role in the pathogenesis of early PD, which is worth further investigation.”
Interdisciplinary collaboration to understand the correlation between the microbiota-gut-brain axis and PD
To understand the correlation between the microbiota-gut-brain axis and the pathogenesis of PD, CU Medicine’s Department of Psychiatry, Department of Microbiology, Division of Neurology, Department of Anatomical and Cellular Pathology, Department of Surgery and Centre for Gut Microbiota Research, and the Center of Parkinsonism and Movement Disorders at the Paracelsus-Elena Hospital in Kassel, Germany, recruited 441 participants, including healthy individuals, RBD patients and their first-degree relatives, and patients with early PD.
Surprisingly, gut microbiome dysbiosis was found in patients with RBD and also among their first-degree relatives, whose microbial compositions have become similar to those of PD patients. This included a depletion of health-promoting bacteria (such as Faecalibacterium and Roseburia) and an increase in bacteria that promote inflammation and disrupt intestinal barrier integrity (such as Collinsella and Akkermansia). These changes cannot be fully explained by constipation symptoms and medications in patients with PD and RBD.
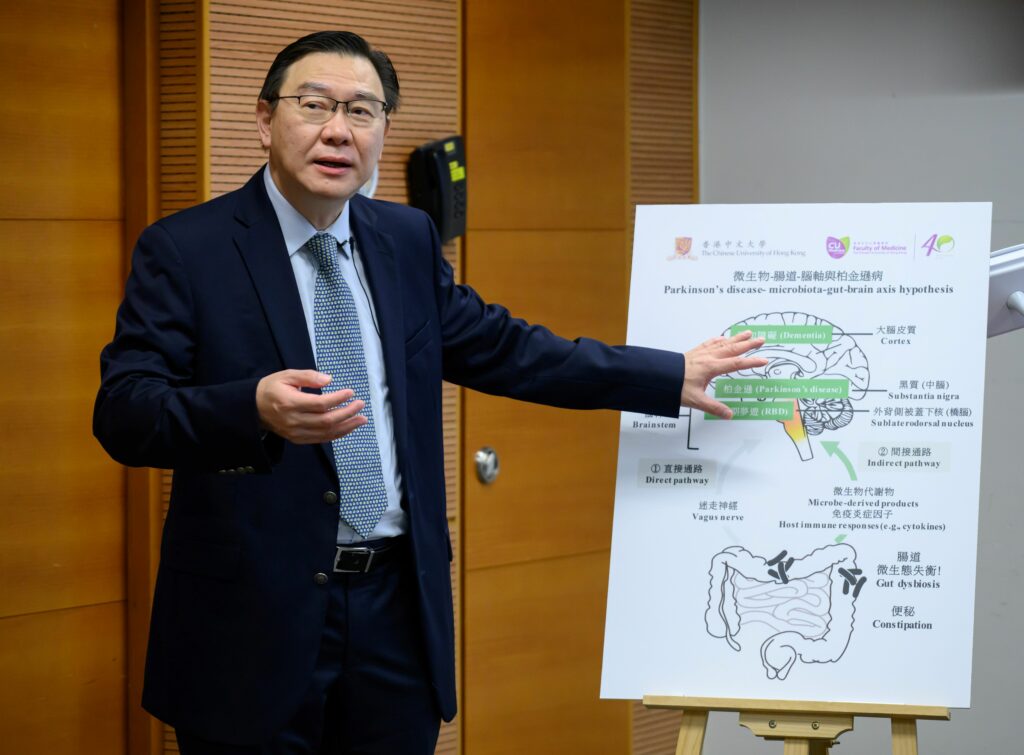
Professor Huang Bei, Research Assistant Professor of CU Medicine’s Department of Psychiatry, explained, “Gut microbiota changes affect the health of both the gut and brain. When the integrity of the intestinal barrier in PD patients is destroyed, it is easier for certain gut metabolites from the microbes and pro-inflammatory factors to enter the nervous system, triggering the abnormal aggregation of synuclein (a neuronal protein) in the enteric nervous system and then progressing into central nervous system, finally leading to neuronal death. This reflects that gut microbiome dysbiosis may be a potential factor leading to Parkinson’s disease.”
Microbial markers are effective in distinguishing RBD from control
Further analysis with machine learning found that 12 microbial markers could effectively distinguish RBD patients from healthy controls. This will facilitate screening of these gut microbial markers to allow early identification of patients with RBD at the prodromal stage of PD. This may reduce their chances of developing PD in the long run through early intervention.
Professor Wing Yun-kwok, Chairman of CU Medicine’s Department of Psychiatry, concluded, “Through the microbiota-gut-brain axis, the gut microbiome influences different physiological conditions such as our sleep, mood, memory and cognitive function. This interdisciplinary study further confirmed that before the onset of PD or even the occurrence of RBD, the patients’ gut ecosystem was disturbed. Restoring healthy gut microbiota, for example by alternating probiotics and prebiotics, may be an early intervention and method of prevention and treatment of PD and other synucelinopathy-related neurodegenerative diseases.”
The original study can be accessed here: https://doi.org/10.1038/s41467-023-38248-4.

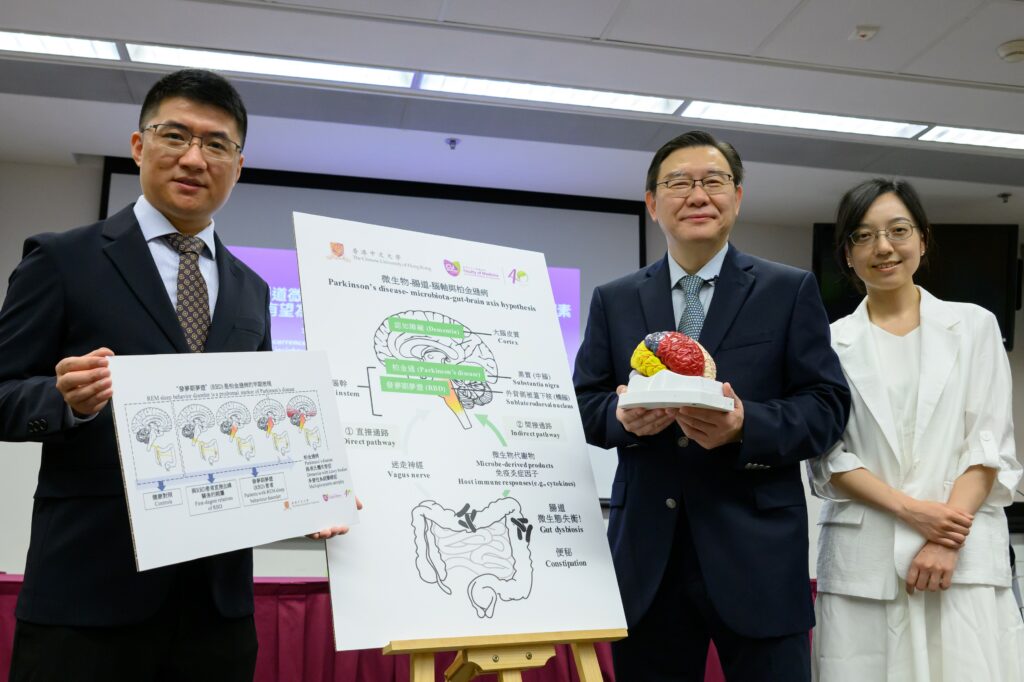
A CU Medicine study discovered that patients with rapid eye movement sleep behaviour disorder (RBD), as well as their first-degree relatives, suffer gut microbiome dysbiosis similar to that of Parkinson’s Disease (PD) patients. This reveals that gut microbiome dysbiosis is a risk factor at the very early stage of PD.
From left: Professor Liu Yaping, Adjunct Assistant Professor; Professor Wing Yun-kwok, Chairman; and Professor Huang Bei, Research Assistant Professor, from the Department of Psychiatry at CU Medicine.
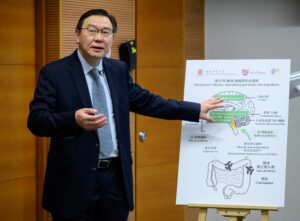
Professor Wing Yun-kwok states that through the microbiota-gut-brain axis, the gut microbiome influences different physiological conditions such as our sleep, mood, memory and cognitive function. Restoring healthy gut microbiota, for example by alternating probiotics and prebiotics, would be an early intervention and method of prevention and treatment of PD and other synucelinopathy-related neurodegenerative diseases.

Professor Huang Bei explains that when the integrity of the intestinal barrier in PD patients is destroyed, it is easier for certain gut metabolites from the microbes and pro-inflammatory factors to enter the nervous system, triggering the abnormal aggregation of synuclein in the enteric nervous system and then progressing into central nervous system, finally leading to neuronal death.