CUHK
News Centre
CU Medicine study identifies 11 allergen components of shrimp for precision diagnosis of shrimp allergy
Shellfish is the most common food allergy, with shrimp being the leading offender, causing symptoms including anaphylaxis in both children and adults. There are several diagnostic approaches to shrimp allergy, such as allergen skin prick tests and measurement of the blood level of the shrimp-specific IgE antibody, but the accuracy is not satisfactory. False-positive rates from these tests can be up to 80 percent.
The Chinese University of Hong Kong’s (CUHK) Faculty of Medicine (CU Medicine) collaborated with Mahidol University and Samitivej Thonburi Hospital in Thailand to study 85 people with shrimp allergy. Researchers collected and analysed serum from them, successfully identifying 11 allergen components of shrimp. The team suggested that the component-based specific IgE antibody test can diagnose shrimp allergy more accurately. They also observed a geographical difference in the prevalence of major allergen components between Hong Kong and Thailand, even though the components were extracted from the same kind of shrimp. This may relate to dietary habits and environmental exposure. The team believes the findings will help promote precision diagnosis of food allergy. Details of the study have been published in authoritative international allergy journal Allergy.
Shrimp is the leading source of food allergy in Hong Kong
Shrimp is the leading source of food allergy in Hong Kong. According to a joint study by CUHK and a number of European and Asian research institutions, the prevalence of probable shrimp allergy among primary schoolchildren in Hong Kong is 1.05%. Patients with shrimp allergy can develop skin reactions and oral symptoms, while it can also lead to wheezing, breathing difficulties and anaphylaxis.
Professor Gary Wong Wing-kin, TS Lo Foundation Professor of Pediatrics from CU Medicine, remarked, “Diagnosis and treatment options for shrimp allergy remain limited. One of the main challenges in managing patients with suspected shrimp allergy is to distinguish between concurrent allergy and asymptomatic sensitisation. If we can nail down the allergen components, we can then develop precision diagnosis and treatment.”
Identifying 11 allergens helps develop precision diagnosis
The study was conducted by researchers from the CUHK Paediatric Allergy team as well as Mahidol University and Samitivej Thonburi Hospital in Bangkok. They recruited 85 people from Hong Kong and Thailand who had experienced immediate allergic reactions after shrimp consumption at least twice within the past five years. Serum was collected to test against the proteins of the giant tiger prawn (Penaeus monodon), which were proved to be a common source of shrimp allergy in southern China in a previous CUHK study. The team successfully identified 11 allergens (see details in Table 1), among which Glycogen phosphorylase (Pen m 14) is newly discovered. They observed a geographical difference in the prevalence of major shrimp allergens between the two populations.
Professor Leung Ting-fan, Alice Ho Miu Ling Nethersole Charity Foundation Professor of Paediatrics from CU Medicine, explained, “Our study essentially provides a comprehensive line-up of shrimp allergens and highlights the diagnostic potential of the relevant components for shrimp allergy management in different geographical populations.”
Component-based specific IgE test could become the gold standard
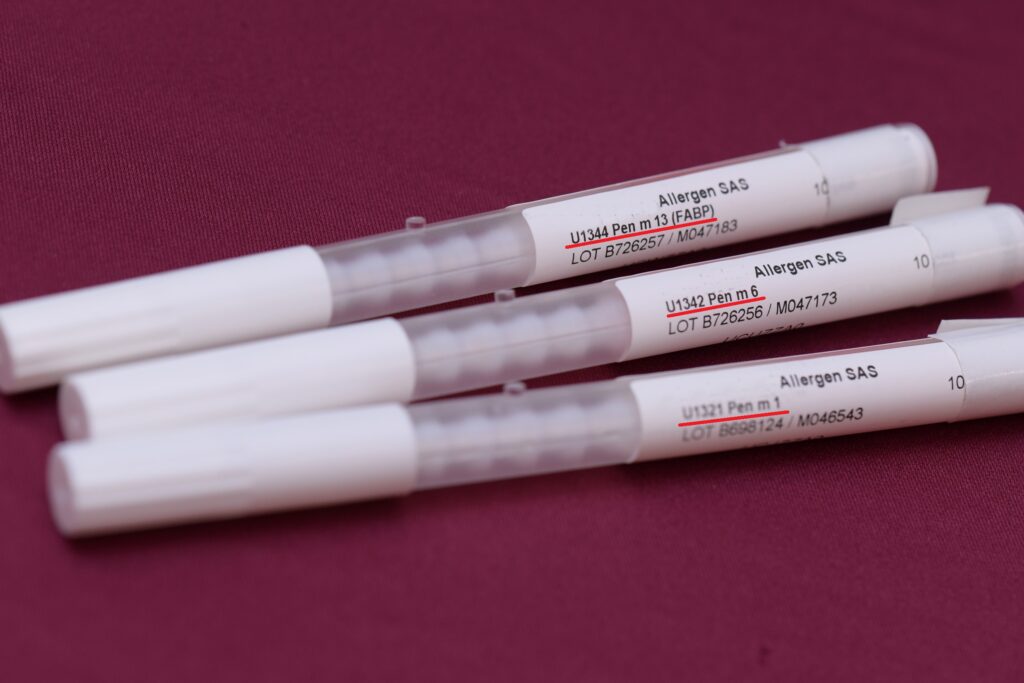
The research team further analysed the IgE reactivity (sensitivity and specificity) of the 11 allergens in shrimp-allergic subjects, and listed the three most useful allergens for shrimp allergy diagnosis in Hong Kong and Thailand separately. (See details in Table 2)
Dr Christine Wai Yee-yan, Research Associate of the Department of Paediatrics at CU Medicine, said, “Conventional skin prick tests and allergen-specific IgE measurement using extract of shellfish for testing lack sufficient accuracy: some food-allergic patients can be mistakenly diagnosed as shrimp-allergic. A double-blind, placebo-controlled food challenge, the existing gold standard for shrimp allergy diagnosis, is risky, labour-intensive and expensive. A component-based specific IgE test can precisely ascertain shrimp allergy, at a lower cost and reduced procedural risk compared to an oral food challenge, meaning it could become the gold standard for diagnosing shrimp allergy in the future.”
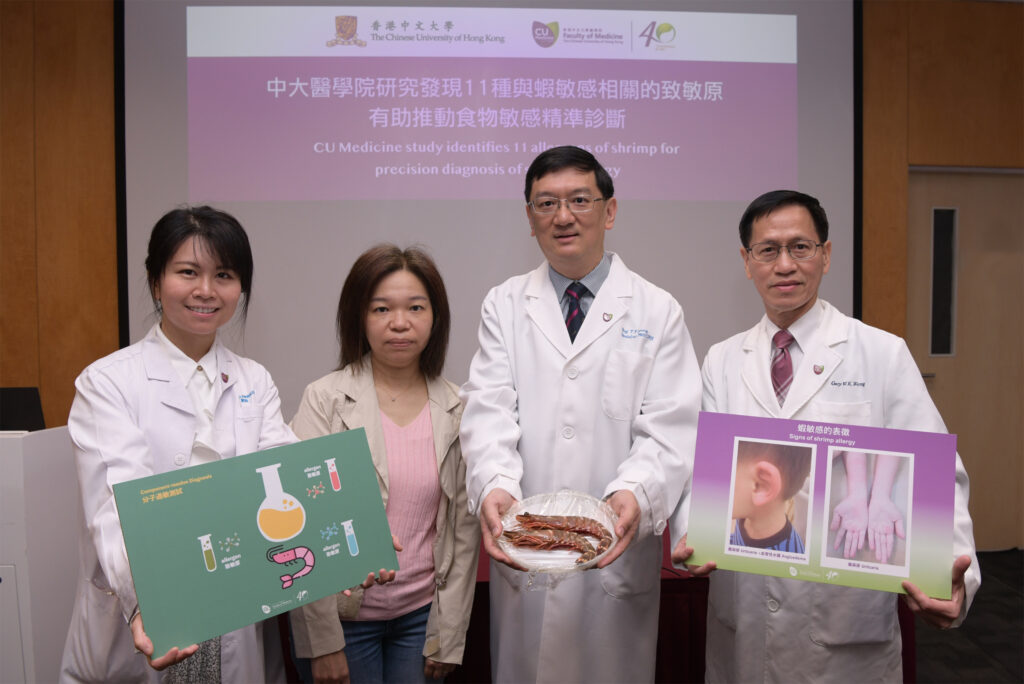
CU Medicine collaborated with Mahidol University and Samitivej Thonburi Hospital in Thailand to study shrimp allergy and successfully identified 11 allergen components of shrimp.
Researchers include Research Associate Dr Christine Wai Yee-yan (1st from left), Alice Ho Miu Ling Nethersole Charity Foundation Professor of Paediatrics Professor Leung Ting-fan (2nd from right) and TS Lo Foundation Professor of Pediatrics Professor Gary Wong Wing-kin from the Department of Paediatrics at CU Medicine (1st from right).

Mrs. Lau’s son Alvin appeared with allergic symptoms after having seafood at around three years old and has stopped consuming seafood since then. When Alvin was 15 years old, CU Medicine tested him with allergen components and found that he is not allergic to shellfish, meaning he can consume scallop or clam.